Oxygen–hemoglobin Dissociation Curve on:
[Wikipedia]
[Google]
[Amazon]
The oxygen–hemoglobin dissociation curve, also called the oxyhemoglobin dissociation curve or oxygen dissociation curve (ODC), is a 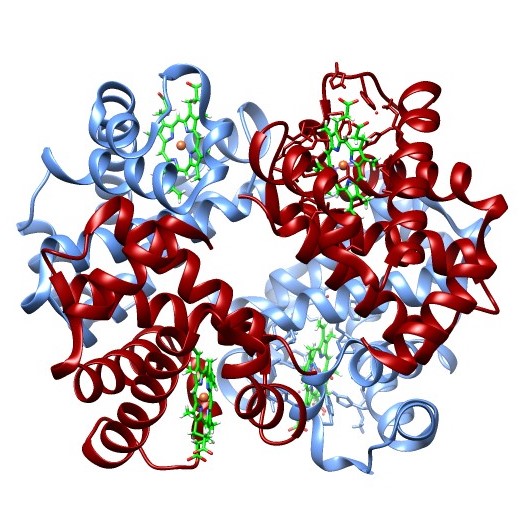
 The curve is usually best described by a
The curve is usually best described by a
Hb-O2 bond), hence, the rightward shift of the curve.

The Interactive Oxyhemoglobin Dissociation Curve
Simulation of the parameters CO2, pH and temperature on the oxygen–hemoglobin dissociation curve (left or right shift)
{{DEFAULTSORT:Oxygen-hemoglobin dissociation curve Respiratory physiology Chemical pathology Hematology Oxygen
curve
In mathematics, a curve (also called a curved line in older texts) is an object similar to a line, but that does not have to be straight.
Intuitively, a curve may be thought of as the trace left by a moving point. This is the definition that ...
that plots the proportion of hemoglobin
Hemoglobin (haemoglobin, Hb or Hgb) is a protein containing iron that facilitates the transportation of oxygen in red blood cells. Almost all vertebrates contain hemoglobin, with the sole exception of the fish family Channichthyidae. Hemoglobin ...
in its saturated (oxygen-laden) form on the vertical axis against the prevailing oxygen tension
Blood gas tension refers to the partial pressure of gases in blood. There are several significant purposes for measuring gas tension. The most common gas tensions measured are oxygen tension (PxO2), carbon dioxide tension (PxCO2) and carbon monoxi ...
on the horizontal axis. This curve is an important tool for understanding how our blood carries and releases oxygen. Specifically, the oxyhemoglobin dissociation curve relates oxygen saturation
Oxygen saturation (symbol SO2) is a relative measure of the concentration of oxygen that is Dissolution (chemistry), dissolved or carried in a given medium as a proportion of the maximal concentration that can be dissolved in that medium at the g ...
(SO2) and partial pressure
In a mixture of gases, each constituent gas has a partial pressure which is the notional pressure of that constituent gas as if it alone occupied the entire volume of the original mixture at the same temperature. The total pressure of an ideal g ...
of oxygen in the blood (PO2), and is determined by what is called "hemoglobin affinity for oxygen"; that is, how readily hemoglobin acquires and releases oxygen molecules into the fluid that surrounds it.
Background
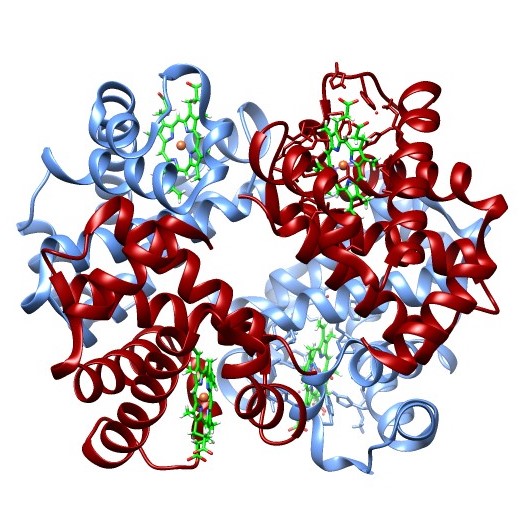
Hemoglobin
Hemoglobin (haemoglobin, Hb or Hgb) is a protein containing iron that facilitates the transportation of oxygen in red blood cells. Almost all vertebrates contain hemoglobin, with the sole exception of the fish family Channichthyidae. Hemoglobin ...
(Hb) is the primary vehicle for transporting oxygen
Oxygen is a chemical element; it has chemical symbol, symbol O and atomic number 8. It is a member of the chalcogen group (periodic table), group in the periodic table, a highly reactivity (chemistry), reactive nonmetal (chemistry), non ...
in the blood
Blood is a body fluid in the circulatory system of humans and other vertebrates that delivers necessary substances such as nutrients and oxygen to the cells, and transports metabolic waste products away from those same cells.
Blood is com ...
. Each hemoglobin molecule has the capacity to carry four oxygen molecules. These molecules of oxygen bind to the globin chain of the heme
Heme (American English), or haem (Commonwealth English, both pronounced /Help:IPA/English, hi:m/ ), is a ring-shaped iron-containing molecule that commonly serves as a Ligand (biochemistry), ligand of various proteins, more notably as a Prostheti ...
prosthetic group
A prosthetic group is the non-amino acid component that is part of the structure of the heteroproteins or conjugated proteins, being tightly linked to the apoprotein.
Not to be confused with the cosubstrate that binds to the enzyme apoenzyme (e ...
.
When hemoglobin has no bound oxygen, nor bound carbon dioxide
Carbon dioxide is a chemical compound with the chemical formula . It is made up of molecules that each have one carbon atom covalent bond, covalently double bonded to two oxygen atoms. It is found in a gas state at room temperature and at norma ...
, it has the unbound conformation (shape). The binding of the first oxygen molecule induces change in the shape of the hemoglobin that increases its ability to bind to the other three oxygen molecules.
In the presence of dissolved carbon dioxide, the pH of the blood changes; this causes another change in the shape of hemoglobin, which increases its ability to bind carbon dioxide and decreases its ability to bind oxygen. With the loss of the first oxygen molecule, and the binding of the first carbon dioxide molecule, yet another change in shape occurs, which further decreases the ability to bind oxygen, and increases the ability to bind carbon dioxide. The oxygen bound to the hemoglobin is released into the blood's plasma and absorbed into the tissues, and the carbon dioxide in the tissues is bound to the hemoglobin.
In the lungs
The lungs are the primary organs of the respiratory system in many animals, including humans. In mammals and most other tetrapods, two lungs are located near the backbone on either side of the heart. Their function in the respiratory syste ...
the reverse of this process takes place. With the loss of the first carbon dioxide molecule the shape again changes and makes it easier to release the other three carbon dioxides.
Oxygen is also carried dissolved in the blood's plasma, but to a much lesser degree. Hemoglobin is contained in red blood cell
Red blood cells (RBCs), referred to as erythrocytes (, with -''cyte'' translated as 'cell' in modern usage) in academia and medical publishing, also known as red cells, erythroid cells, and rarely haematids, are the most common type of blood cel ...
s. Hemoglobin releases the bound oxygen when carbonic acid
Carbonic acid is a chemical compound with the chemical formula . The molecule rapidly converts to water and carbon dioxide in the presence of water. However, in the absence of water, it is quite stable at room temperature. The interconversion ...
is present, as it is in the tissues. In the capillaries
A capillary is a small blood vessel, from 5 to 10 micrometres in diameter, and is part of the microcirculation system. Capillaries are microvessels and the smallest blood vessels in the body. They are composed of only the tunica intima (the in ...
, where carbon dioxide
Carbon dioxide is a chemical compound with the chemical formula . It is made up of molecules that each have one carbon atom covalent bond, covalently double bonded to two oxygen atoms. It is found in a gas state at room temperature and at norma ...
is produced, oxygen bound to the hemoglobin is released into the blood's plasma and absorbed into the tissues.
How much of that capacity is filled by oxygen at any time is called the oxygen saturation
Oxygen saturation (symbol SO2) is a relative measure of the concentration of oxygen that is Dissolution (chemistry), dissolved or carried in a given medium as a proportion of the maximal concentration that can be dissolved in that medium at the g ...
. Expressed as a percentage, the oxygen saturation is the ratio of the amount of oxygen bound to the hemoglobin, to the oxygen-carrying capacity of the hemoglobin. The oxygen-carrying capacity of hemoglobin is determined by the type of hemoglobin present in the blood. The amount of oxygen bound to the hemoglobin at any time is related, in large part, to the partial pressure
In a mixture of gases, each constituent gas has a partial pressure which is the notional pressure of that constituent gas as if it alone occupied the entire volume of the original mixture at the same temperature. The total pressure of an ideal g ...
of oxygen to which the hemoglobin is exposed. In the lungs, at the alveolar–capillary interface, the partial pressure of oxygen is typically high, and therefore the oxygen binds readily to hemoglobin that is present. As the blood circulates to other body tissue in which the partial pressure of oxygen is less, the hemoglobin releases the oxygen into the tissue because the hemoglobin cannot maintain its full bound capacity of oxygen in the presence of lower oxygen partial pressures.
Sigmoid shape
 The curve is usually best described by a
The curve is usually best described by a sigmoid
Sigmoid means resembling the lower-case Greek letter sigma (uppercase Σ, lowercase σ, lowercase in word-final position ς) or the Latin letter S. Specific uses include:
* Sigmoid function, a mathematical function
* Sigmoid colon, part of the l ...
plot, using a formula of the kind:
:
A hemoglobin molecule can bind up to four oxygen molecules in a reversible method.
The shape of the curve results from the interaction of bound oxygen molecules with incoming molecules. The binding of the first molecule is difficult. However, this facilitates the binding of the second, third and fourth, this is due to the induced conformational change in the structure of the hemoglobin molecule induced by the binding of an oxygen molecule.
In its simplest form, the oxyhemoglobin dissociation curve describes the relation between the partial pressure of oxygen (x axis) and the oxygen saturation (y axis). Hemoglobin's affinity for oxygen increases as successive molecules of oxygen bind. More molecules bind as the oxygen partial pressure increases until the maximum amount that can be bound is reached. As this limit is approached, very little additional binding occurs and the curve levels out as the hemoglobin becomes saturated with oxygen. Hence the curve has a sigmoidal or S-shape. At pressures above about 60 mmHg, the standard dissociation curve is relatively flat, which means that the oxygen content of the blood does not change significantly even with large increases in the oxygen partial pressure. To get more oxygen to the tissue would require blood transfusions to increase the hemoglobin count (and hence the oxygen-carrying capacity), or supplemental oxygen that would increase the oxygen dissolved in plasma.
Although binding of oxygen to hemoglobin continues to some extent for pressures about 50 mmHg, as oxygen partial pressures decrease in this steep area of the curve, the oxygen is unloaded to peripheral tissue readily as the hemoglobin's affinity diminishes.
The partial pressure of oxygen in the blood at which the hemoglobin is 50% saturated, typically about 26.6 mmHg (3.5 kPa) for a healthy person, is known as the P50. The P50 is a conventional measure of hemoglobin affinity for oxygen. In the presence of disease or other conditions that change the hemoglobin oxygen affinity and, consequently, shift the curve to the right or left, the P50 changes accordingly. An increased P50 indicates a rightward shift of the standard curve, which means that a larger partial pressure is necessary to maintain a 50% oxygen saturation. This indicates a decreased affinity. Conversely, a lower P50 indicates a leftward shift and a higher affinity.
The 'plateau' portion of the oxyhemoglobin dissociation curve is the range that exists at the pulmonary capillaries (minimal reduction of oxygen transported until the p(O2) falls 50 mmHg).
The 'steep' portion of the oxyhemoglobin dissociation curve is the range that exists at the systemic capillaries (a small drop in systemic capillary p(O2) can result in the release of large amounts of oxygen for the metabolically active cells).
To see the relative affinities of each successive oxygen as you remove/add oxygen from/to the hemoglobin from the curve compare the relative increase/decrease in p(O2) needed for the corresponding increase/decrease in s(O2).
Factors that affect the standard dissociation curve
The strength with which oxygen binds to hemoglobin is affected by several factors. These factors shift or reshape the oxyhemoglobin dissociation curve. A shift to right indicates that the hemoglobin under study has a decreased affinity for oxygen. This makes it more difficult for hemoglobin to bind to oxygen (requiring a higher partial pressure of oxygen to achieve the same oxygen saturation), but it makes it easier for the hemoglobin to release oxygen bound to it. The effect of this shift of the curve increases the partial pressure of oxygen in the tissues when it is most needed, such as during exercise, or hemorrhagic shock. In contrast, the curve is shifted to the left by the opposite of these conditions. This shift indicates that the hemoglobin under study has an increased affinity for oxygen so that hemoglobin binds oxygen more easily, but unloads it more reluctantly. Left shift of the curve is a sign of hemoglobin's increased affinity for oxygen (e.g. at the lungs). Similarly, right shift shows decreased affinity, as would appear with an increase in either body temperature, hydrogen ions,2,3-bisphosphoglycerate
2,3-Bisphosphoglyceric acid (conjugate base 2,3-bisphosphoglycerate) (2,3-BPG), also known as 2,3-diphosphoglyceric acid (conjugate base 2,3-diphosphoglycerate) (2,3-DPG), is a three-carbon isomer of the glycolytic intermediate 1,3-bisphosphoglyc ...
(2,3-BPG) concentration or carbon dioxide concentration.
Note:
* Left shift: higher O2 affinity
* Right shift: lower O2 affinity
* fetal hemoglobin has higher O2 affinity than adult hemoglobin; primarily due to much-reduced affinity to 2,3-bisphosphoglycerate
2,3-Bisphosphoglyceric acid (conjugate base 2,3-bisphosphoglycerate) (2,3-BPG), also known as 2,3-diphosphoglyceric acid (conjugate base 2,3-diphosphoglycerate) (2,3-DPG), is a three-carbon isomer of the glycolytic intermediate 1,3-bisphosphoglyc ...
.
The causes of shift to right can be remembered using the mnemonic
A mnemonic device ( ), memory trick or memory device is any learning technique that aids information retention or retrieval in the human memory, often by associating the information with something that is easier to remember.
It makes use of e ...
, "CADET, face Right!" for CO2, Acid, 2,3-DPG, Exercise and Temperature. Factors that move the oxygen dissociation curve to the right are those physiological states where tissues need more oxygen. For example, during exercise, muscles have a higher metabolic rate, and consequently need more oxygen, produce more carbon dioxide and lactic acid, and their temperature rises.
pH
A decrease in pH (increase in ion concentration) shifts the standard curve to the right, while an increase shifts it to the left. This occurs because at greater ion concentration, various amino acid residues, such as Histidine 146 exist predominantly in their protonated form allowing them to form ion pairs that stabilize deoxyhemoglobin in the T state. The T state has a lower affinity for oxygen than the R state, so with increased acidity, the hemoglobin binds less O2 for a given PO2 (and more H+). This is known as theBohr effect
The Bohr effect is a phenomenon first described in 1904 by the Danish physiologist Christian Bohr. Hemoglobin's oxygen binding affinity (see oxygen–haemoglobin dissociation curve) is inversely related both to acidity and to the concentration of ...
. A reduction in the total binding capacity of hemoglobin to oxygen (i.e. shifting the curve down, not just to the right) due to reduced pH is called the root effect. This is seen in bony fish. The binding affinity of hemoglobin to O2 is greatest under a relatively high pH.
Carbon dioxide
Carbon dioxide
Carbon dioxide is a chemical compound with the chemical formula . It is made up of molecules that each have one carbon atom covalent bond, covalently double bonded to two oxygen atoms. It is found in a gas state at room temperature and at norma ...
affects the curve in two ways. First, CO2 accumulation causes carbamino
Carbamino refers to an adduct generated by the addition of carbon dioxide to the free amino group of an amino acid or a protein, such as hemoglobin forming carbaminohemoglobin.
Determining quantity of carboamino in products
It is possible to det ...
compounds to be generated through chemical interactions, which bind to hemoglobin forming carbaminohemoglobin
Carbaminohemoglobin (carbaminohaemoglobin BrE) (CO2Hb, also known as carbhemoglobin and carbohemoglobin) is a Chemical compound, compound of hemoglobin and carbon dioxide, and is one of the forms in which carbon dioxide exists in the blood. In bl ...
. CO2 is considered an Allosteric regulation
In the fields of biochemistry and pharmacology an allosteric regulator (or allosteric modulator) is a substance that binds to a site on an enzyme or receptor distinct from the active site, resulting in a conformational change that alters the ...
as the inhibition happens not at the binding site of hemoglobin. Second, it influences intracellular pH
Intracellular pH (pHi) is the measure of the acidity or basicity (i.e., pH) of intracellular fluid. The pHi plays a critical role in membrane transport and other intracellular processes. In an environment with the improper pHi, biological cells m ...
due to formation of bicarbonate ion. Formation of carbaminohemoglobin stabilizes T state hemoglobin by formation of ion pairs. Only about 5–10% of the total CO2 content of blood is transported as carbamino compounds, whereas (80–90%) is transported as bicarbonate ions and a small amount is dissolved in the plasma. The formation of a bicarbonate ion will release a proton into the plasma, decreasing pH (increased acidity), which also shifts the curve to the right as discussed above; low CO2 levels in the blood stream results in a high pH, and thus provides more optimal binding conditions for hemoglobin and O2. This is a physiologically favored mechanism, since hemoglobin will drop off more oxygen as the concentration of carbon dioxide increases dramatically where tissue respiration is happening rapidly and oxygen is in need.
2,3-BPG
2,3-Bisphosphoglycerate or 2,3-BPG (formerly named 2,3-diphosphoglycerate or 2,3-DPG) is anorganophosphate
In organic chemistry, organophosphates (also known as phosphate esters, or OPEs) are a class of organophosphorus compounds with the general structure , a central phosphate molecule with alkyl or aromatic substituents. They can be considered ...
formed in red blood cell
Red blood cells (RBCs), referred to as erythrocytes (, with -''cyte'' translated as 'cell' in modern usage) in academia and medical publishing, also known as red cells, erythroid cells, and rarely haematids, are the most common type of blood cel ...
s during glycolysis
Glycolysis is the metabolic pathway that converts glucose () into pyruvic acid, pyruvate and, in most organisms, occurs in the liquid part of cells (the cytosol). The Thermodynamic free energy, free energy released in this process is used to form ...
and is the conjugate base
A conjugate acid, within the Brønsted–Lowry acid–base theory, is a chemical compound formed when an acid gives a proton () to a base—in other words, it is a base with a hydrogen ion added to it, as it loses a hydrogen ion in the reve ...
of 2,3-bisphosphoglyceric acid
2,3-Bisphosphoglyceric acid (conjugate base 2,3-bisphosphoglycerate) (2,3-BPG), also known as 2,3-diphosphoglyceric acid (conjugate base 2,3-diphosphoglycerate) (2,3-DPG), is a three-carbon isomer of the glycolytic intermediate 1,3-bisphosphoglyc ...
. The production of 2,3-BPG is likely an important adaptive mechanism, because the production increases for several conditions in the presence of diminished peripheral tissue O2 availability, such as hypoxemia
Hypoxemia (also spelled hypoxaemia) is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia is usually caused by pulmonary disease. Sometimes the concentration of oxygen in the ...
, chronic lung disease, anemia
Anemia (also spelt anaemia in British English) is a blood disorder in which the blood has a reduced ability to carry oxygen. This can be due to a lower than normal number of red blood cells, a reduction in the amount of hemoglobin availabl ...
, and congestive heart failure
Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome caused by an impairment in the heart's ability to fill with and pump blood.
Although symptoms vary based on which side of the heart is affected, HF typically pr ...
, among others, which necessitate easier oxygen unloading in the peripheral tissue. High levels of 2,3-BPG shift the curve to the right (as in childhood), while low levels of 2,3-BPG cause a leftward shift, seen in states such as septic shock
Septic shock is a potentially fatal medical condition that occurs when sepsis, which is organ injury or damage in response to infection, leads to dangerously low blood pressure and abnormalities in cellular metabolism. The Third International C ...
, and hypophosphataemia. In the absence of 2,3-BPG, hemoglobin's affinity for oxygen increases. 2,3-BPG acts as a heteroallosteric effector of hemoglobin, lowering hemoglobin's affinity for oxygen by binding preferentially to deoxyhemoglobin. An increased concentration of BPG in red blood cells favours formation of the T (taut or tense), low-affinity state of hemoglobin and so the oxygen-binding curve will shift to the right.
Temperature
Increase in temperature shifts the oxygen dissociation curve to the right. When temperature is increased keeping the oxygen concentration constant, oxygen saturation decreases as the bond between oxygen and iron gets denatured. Additionally, with increased temperature, the partial pressure of oxygen increases as well. So, one will have a lesser amount of hemoglobin saturated for the same oxygen concentration but at a higher partial pressure of oxygen. Thus, any point in the curve will shift rightwards (due to increased partial pressure of oxygen) and downwards (due to weakenedCarbon monoxide
Hemoglobin binds withcarbon monoxide
Carbon monoxide (chemical formula CO) is a poisonous, flammable gas that is colorless, odorless, tasteless, and slightly less dense than air. Carbon monoxide consists of one carbon atom and one oxygen atom connected by a triple bond. It is the si ...
210 times more readily than with oxygen. Because of this higher affinity of hemoglobin for carbon monoxide than for oxygen, carbon monoxide is a highly successful competitor that will displace oxygen even at minuscule partial pressures. The reaction HbO2 + CO → HbCO + O2 almost irreversibly displaces the oxygen molecules forming carboxyhemoglobin
Carboxyhemoglobin (carboxyhaemoglobin BrE) (symbol COHb or HbCO) is a stable complex (chemistry), complex of carbon monoxide and hemoglobin (Hb) that forms in red blood cells upon contact with carbon monoxide. Carboxyhemoglobin is often mistaken ...
; the binding of the carbon monoxide to the iron centre of hemoglobin is much stronger than that of oxygen, and the binding site remains blocked for the remainder of the life cycle of that affected red blood cell. With an increased level of carbon monoxide, a person can suffer from severe tissue hypoxia while maintaining a normal pO2 because carboxyhemoglobin does not carry oxygen to the tissues.
Effects of methemoglobinaemia
Methemoglobinaemia is a form of abnormal hemoglobin where the iron centre has been oxidised from the ferrous +2oxidation state
In chemistry, the oxidation state, or oxidation number, is the hypothetical Electrical charge, charge of an atom if all of its Chemical bond, bonds to other atoms are fully Ionic bond, ionic. It describes the degree of oxidation (loss of electrons ...
(the normal form, which on binding with oxygen changes to the ferric state) to the ferric +3 state. This causes a leftward shift in the oxygen hemoglobin dissociation curve, as any residual heme with oxygenated ferrous iron (+2 state) is unable to unload its bound oxygen into tissues (because 3+ iron impairs hemoglobin's cooperativity), thereby increasing its affinity with oxygen. However, methemoglobin has increased affinity for cyanide
In chemistry, cyanide () is an inorganic chemical compound that contains a functional group. This group, known as the cyano group, consists of a carbon atom triple-bonded to a nitrogen atom.
Ionic cyanides contain the cyanide anion . This a ...
, and is therefore useful in the treatment of cyanide poisoning
Cyanide poisoning is poisoning that results from exposure to any of a number of forms of cyanide. Early symptoms include headache, dizziness, fast heart rate, shortness of breath, and vomiting. This phase may then be followed by seizures, slo ...
. In cases of accidental ingestion, administration of a nitrite
The nitrite polyatomic ion, ion has the chemical formula . Nitrite (mostly sodium nitrite) is widely used throughout chemical and pharmaceutical industries. The nitrite anion is a pervasive intermediate in the nitrogen cycle in nature. The name ...
(such as amyl nitrite
Amyl nitrite is a chemical compound with the formula C5H11ONO. A variety of isomers are known, but they all feature an amyl group attached to the nitrite functional group. The alkyl group (the amyl in this case) is unreactive and the chemical ...
) can be used to deliberately oxidise hemoglobin and raise methemoglobin levels, restoring the functioning of cytochrome oxidase
The enzyme cytochrome c oxidase or Complex IV (was , now reclassified as a translocasEC 7.1.1.9 is a large transmembrane protein complex found in bacteria, archaea, and the mitochondria of eukaryotes.
It is the last enzyme in the respiratory e ...
. The nitrite also acts as a vasodilator
Vasodilation, also known as vasorelaxation, is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. Blood vessel wal ...
, promoting the cellular supply of oxygen, and the addition of an iron salt provides for competitive binding of the free cyanide as the biochemically inert hexacyanoferrate(III)
Ferricyanide is the name of the anion
ion, e(CN)6sup>3−. An alternative approach involves administering e(cyanide, CN)6
E, or e, is the fifth letter and the second vowel letter of the Latin alphabet, used in the modern English alphabet, the alphabets of other western European languages and others worldwide. Its name in English is ''e'' (pronounced ); plur ...
−. It is also called hexacyanoferrate(III) and in rare, but systematic name, systematic nomenclature, hexacyanidoferrate(III). The most common salt of this anion is potassium ferricyanid ...thiosulfate
Thiosulfate ( IUPAC-recommended spelling; sometimes thiosulphate in British English) is an oxyanion of sulfur with the chemical formula . Thiosulfate also refers to the compounds containing this anion, which are the salts of thiosulfuric acid, ...
, thereby converting cyanide to thiocyanate
Thiocyanates are salts containing the thiocyanate anion (also known as rhodanide or rhodanate). is the conjugate base of thiocyanic acid. Common salts include the colourless salts potassium thiocyanate and sodium thiocyanate. Mercury(II) t ...
, SCN−, which is excreted ''via'' the kidneys. Methemoglobin is also formed in small quantities when the dissociation of oxyhemoglobin results in the formation of methemoglobin and superoxide
In chemistry, a superoxide is a compound that contains the superoxide ion, which has the chemical formula . The systematic name of the anion is dioxide(1−). The reactive oxygen ion superoxide is particularly important as the product of t ...
, O2−, instead of the usual products. Superoxide is a free radical
A daughter category of ''Ageing'', this category deals only with the biological aspects of ageing.
Ageing
Biogerontology
Biological processes
Causes of death
Cellular processes
Gerontology
Life extension
Metabolic disorders
Metabolism
...
and causes biochemical damage, but is neutralised by the action of the enzyme superoxide dismutase
Superoxide dismutase (SOD, ) is an enzyme that alternately catalyzes the dismutation (or partitioning) of the superoxide () anion radical into normal molecular oxygen (O2) and hydrogen peroxide (). Superoxide is produced as a by-product of oxy ...
.
Effects of ITPP
Myo-inositol trispyrophosphate (ITPP), also known as OXY111A, is aninositol phosphate
Inositol phosphates are a group of mono- to hexaphosphorylated inositols. Each form of inositol phosphate is distinguished by the number and position of the phosphate group on the inositol ring.
* inositol monophosphate (IP)
* inositol bisphospha ...
that causes a rightward shift in the oxygen hemoglobin dissociation curve through allosteric modulation of hemoglobin within red blood cells. It is an experimental drug intended to reduce tissue hypoxia. The effects appear to last roughly as long as the affected red blood cells remain in circulation.
Fetal hemoglobin

Fetal hemoglobin
Fetal hemoglobin, or foetal haemoglobin (also hemoglobin F, HbF, or α2γ2) is the main oxygen carrier protein in the human fetus. HemoglobinF is found in fetal red blood cells, and is involved in transporting oxygen from the mother's bloodstream ...
(HbF) is structurally different from normal adult hemoglobin
Hemoglobin A (HbA), also known as adult hemoglobin, hemoglobin A1 or α2β2, is the most common human hemoglobin tetramer, accounting for over 97% of the total red blood cell hemoglobin. Hemoglobin is an oxygen-binding protein, found in erythrocyt ...
(HbA), giving HbF a higher affinity for oxygen than HbA. HbF is composed of two alpha and two gamma chains, whereas HbA is composed of two alpha and two beta chains. The fetal dissociation curve is shifted to the left relative to the curve for the normal adult because of these structural differences:
In adult hemoglobin, the binding of 2,3-bisphosphoglycerate (2,3-BPG) primarily occurs with the beta chains, preventing the binding of oxygen with haemoglobin. This binding is crucial for stabilizing the deoxygenated state of hemoglobin, promoting the efficient release of oxygen to body tissues.
In fetal hemoglobin, which possesses a gamma chain instead of a beta chain, the interaction with 2,3-BPG differs because 2,3-BPG does not bind with the gamma chain as it has lower to no affinity with the gamma chain. This distinction contributes to fetal hemoglobin having a higher affinity for oxygen.
Typically, fetal arterial oxygen pressures are lower than adult arterial oxygen pressures. Hence, higher affinity to bind oxygen is required at lower levels of partial pressure in the fetus to allow diffusion of oxygen across the placenta
The placenta (: placentas or placentae) is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas, and waste exchange between ...
. At the placenta, there is a higher concentration of 2,3-BPG formed, and 2,3-BPG binds readily to beta chains rather than to alpha chains. As a result, 2,3-BPG binds more strongly to adult hemoglobin, causing HbA to release more oxygen for uptake by the fetus, whose HbF is unaffected by the 2,3-BPG. HbF then delivers that bound oxygen to tissues that have even lower partial pressures where it can be released.
See also
*Automated analyzer
An automated analyser is a medical laboratory instrument designed to measure various substances and other characteristics in a number of biological Sample (material), samples quickly, with minimal human assistance. These measured properties of bloo ...
* Bohr effect
The Bohr effect is a phenomenon first described in 1904 by the Danish physiologist Christian Bohr. Hemoglobin's oxygen binding affinity (see oxygen–haemoglobin dissociation curve) is inversely related both to acidity and to the concentration of ...
Notes
References
External links
*The Interactive Oxyhemoglobin Dissociation Curve
Simulation of the parameters CO2, pH and temperature on the oxygen–hemoglobin dissociation curve (left or right shift)
{{DEFAULTSORT:Oxygen-hemoglobin dissociation curve Respiratory physiology Chemical pathology Hematology Oxygen