Monoparesis on:
[Wikipedia]
[Google]
[Amazon]
Monoplegia is
 In monoplegia, the spine and the proximal portion of nerves are usually the abnormal sites of limb weakness. Monoplegia resulting from upper extremity impairments following a stroke occurs due to direct damage to the
In monoplegia, the spine and the proximal portion of nerves are usually the abnormal sites of limb weakness. Monoplegia resulting from upper extremity impairments following a stroke occurs due to direct damage to the
paralysis
Paralysis (also known as plegia) is a loss of motor function in one or more muscles. Paralysis can also be accompanied by a loss of feeling (sensory loss) in the affected area if there is sensory damage. In the United States, roughly 1 in 50 ...
of a single limb
Limb may refer to:
Science and technology
*Limb (anatomy), an appendage of a human or animal
*Limb, a large or main branch of a tree
*Limb, in astronomy, the curved edge of the apparent disk of a celestial body, e.g. lunar limb
*Limb, in botany, ...
, usually an arm. Common symptoms associated with monoplegic patients are weakness, numbness, and pain in the affected limb. Monoplegia is a type of paralysis that falls under hemiplegia
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body ('' hemi-'' means "half"). Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medic ...
. While hemiplegia is paralysis of half of the body, monoplegia is localized to a single limb or to a specific region of the body. Monoplegia of the upper limb is sometimes referred to as brachial monoplegia, and that of the lower limb is called crural monoplegia. Monoplegia in the lower extremities is not as common of an occurrence as in the upper extremities. Monoparesis is a similar, but less severe, condition because one limb is very weak, not paralyzed. For more information, see paresis
In medicine, paresis () is a condition typified by a weakness of voluntary movement, or by partial loss of voluntary movement or by impaired movement. When used without qualifiers, it usually refers to the limbs, but it can also be used to desc ...
.
Many conditions that cause paraplegia
Paraplegia, or paraparesis, is an impairment in motor or sensory function of the lower extremities. The word comes from Ionic Greek ()
"half-stricken". It is usually caused by spinal cord injury or a congenital condition that affects the neural ...
or quadriplegia begin as monoplegia. Thus, the diagnosis of spinal paraplegia
Paraplegia, or paraparesis, is an impairment in motor or sensory function of the lower extremities. The word comes from Ionic Greek ()
"half-stricken". It is usually caused by spinal cord injury or a congenital condition that affects the neural ...
must also be consulted. In addition, multiple cerebral disorders that cause hemiplegia
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body ('' hemi-'' means "half"). Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medic ...
may begin as monoplegia. Monoplegia is also frequently associated with, and considered to be the mildest form of, cerebral palsy
Cerebral palsy (CP) is a group of movement disorders that appear in early childhood. Signs and symptoms vary among people and over time, but include poor coordination, stiff muscles, weak muscles, and tremors. There may be problems with sensa ...
.
Signs and symptoms
There are a number of symptoms associated with monoplegia. Curling of the hands or stiffness of the feet, weakness,spasticity
Spasticity () is a feature of altered skeletal muscle performance with a combination of paralysis, increased tendon reflex activity, and hypertonia. It is also colloquially referred to as an unusual "tightness", stiffness, or "pull" of muscles.
...
, numbness, paralysis, pain in the affected limb, headaches, and shoulder pain are all considered to be symptoms of monoplegia. Patients of monoplegia typically feel symptoms of weakness and loss of sensation in the affected extremity, usually an arm. Despite these symptoms, the extremity with paralysis continues to maintain a strong pulse.
While chronic progressive brachial monoplegia is uncommon, syringomyelia
Syringomyelia is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. Often, syringomyelia is used as a generic term before an etiology is determined. This cyst, called a syrinx, can expand and elongate ...
and tumors of the cervical cord or brachial plexus
The brachial plexus is a network () of nerves formed by the anterior rami of the lower four cervical nerves and first thoracic nerve ( C5, C6, C7, C8, and T1). This plexus extends from the spinal cord, through the cervicoaxillary canal in th ...
may be the cause. The onset of brachial plexus paralysis is usually explosive where pain is the initial feature. Pain localizes to the shoulder but may be more diffuse, or could be limited to the lower arm. Pain is severe and often described as sharp, stabbing, throbbing, or aching. The duration of pain, which is constant, varies from a span of several hours to 3 weeks. As the pain subsides, weakness usually appears. In addition, chronicle progressive weakness of one leg suggests a tumor of the spinal cord of the lumbar plexus
The lumbar plexus is a web of nerves (a nervous plexus) in the lumbar region of the body which forms part of the larger lumbosacral plexus. It is formed by the Ventral ramus of spinal nerve, divisions of the first four lumbar nerves (L1-L4) and ...
. Fever is often the first symptom of lumbar plexus paralysis, followed by pain in one or both legs. The pain has an abrupt onset and may occur in a femoral or sciatic
The sciatic nerve, also called the ischiadic nerve, is a large nerve in humans and other vertebrate animals which is the largest branch of the sacral plexus and runs alongside the hip joint and down the lower limb. It is the longest and widest si ...
distribution. Weakness may develop concurrently with pain or be delayed for as long as 3 weeks. Furthermore, a monomeric form of spinal muscular atrophy
Spinal muscular atrophy (SMA) is a rare neuromuscular disorder that results in the loss of motor neurons and progressive muscle wasting. It is usually diagnosed in infancy or early childhood and if left untreated it is the most common genetic ...
, affecting only one leg or arm, should be considered when progressive weakness is not accompanied by sensory loss.
Causes
Some potential causes of monoplegia are listed below. # Cerebral palsy # Direct physical trauma to the affected limb # Central nervous mass lesion, includingtumor
A neoplasm () is a type of abnormal and excessive growth of tissue. The process that occurs to form or produce a neoplasm is called neoplasia. The growth of a neoplasm is uncoordinated with that of the normal surrounding tissue, and persists ...
, hematoma
A hematoma, also spelled haematoma, or blood suffusion is a localized bleeding outside of blood vessels, due to either disease or trauma including injury or surgery and may involve blood continuing to seep from broken capillary, capillaries. A he ...
, or abscess
An abscess is a collection of pus that has built up within the tissue of the body. Signs and symptoms of abscesses include redness, pain, warmth, and swelling. The swelling may feel fluid-filled when pressed. The area of redness often extends b ...
# Complicated migraine
Migraine (, ) is a common neurological disorder characterized by recurrent headaches. Typically, the associated headache affects one side of the head, is pulsating in nature, may be moderate to severe in intensity, and could last from a few hou ...
# Epilepsy
Epilepsy is a group of non-communicable neurological disorders characterized by recurrent epileptic seizures. Epileptic seizures can vary from brief and nearly undetectable periods to long periods of vigorous shaking due to abnormal electrical ...
# Head or spinal trauma
# Hereditary brachial neuritis Brachial means "pertaining to the arm", and may refer to:
* Brachial artery, in anatomy
* Brachial fascia
* Brachial lymph nodes
* Brachial veins
* Brachial plexus, a network of nerves
* Brachial valve, the upper valve in Brachiopods
* Brachiali ...
# Hereditary neuropathy
Peripheral neuropathy, often shortened to neuropathy, is a general term describing disease affecting the peripheral nerves, meaning nerves beyond the brain and spinal cord. Damage to peripheral nerves may impair sensation, movement, gland, or o ...
with liability to pressure palsy
# Neonatal brachial plexus
The brachial plexus is a network () of nerves formed by the anterior rami of the lower four cervical nerves and first thoracic nerve ( C5, C6, C7, C8, and T1). This plexus extends from the spinal cord, through the cervicoaxillary canal in th ...
paralysis
# Neuropathy
Peripheral neuropathy, often shortened to neuropathy, is a general term describing disease affecting the peripheral nerves, meaning nerves beyond the brain and spinal cord. Damage to peripheral nerves may impair sensation, movement, gland, or o ...
# Plexopathy Plexopathy is a disorder of the wikt:network, network of nerves in the brachial plexus, brachial or lumbosacral plexus. Symptoms include pain, muscle weakness, and sensory deficits (numbness).
Types
There are two main types of plexopathy, based on ...
# Traumatic peroneal neuropathy
# Vaccine-associated paralytic poliomyelitis
# Hemiparetic seizures
# Monomeric spinal muscular atrophy
# Stroke
A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functionin ...
Specifically, monoplegia in the lower extremities is typically caused by Brown Sequard syndrome and hematomas in the frontoparietal cortex near the middle that could produce a deficit such as this, but this is a very uncommon occurrence.
Mechanism
 In monoplegia, the spine and the proximal portion of nerves are usually the abnormal sites of limb weakness. Monoplegia resulting from upper extremity impairments following a stroke occurs due to direct damage to the
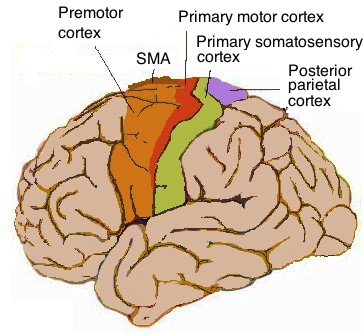
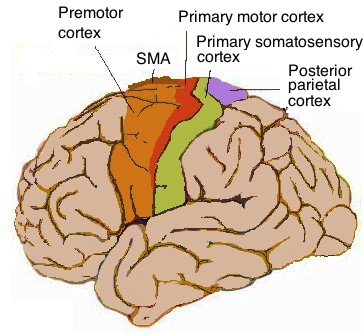
In monoplegia, the spine and the proximal portion of nerves are usually the abnormal sites of limb weakness. Monoplegia resulting from upper extremity impairments following a stroke occurs due to direct damage to the primary motor cortex
The primary motor cortex (Brodmann area 4) is a brain region that in humans is located in the dorsal portion of the frontal lobe. It is the primary region of the motor system and works in association with other motor areas including premotor co ...
, primary somatosensory cortex
In neuroanatomy, the primary somatosensory cortex is located in the postcentral gyrus of the brain's parietal lobe, and is part of the somatosensory system. It was initially defined from surface stimulation studies of Wilder Penfield, and paralle ...
, secondary sensorimotor cortex
The motor cortex is the region of the cerebral cortex believed to be involved in the planning, control, and execution of voluntary movements.
The motor cortex is an area of the frontal lobe located in the posterior precentral gyrus immediately ...
, sensorimotor cortical areas, subcortical structures, and/or the corticospinal tract
The corticospinal tract is a white matter motor pathway starting at the cerebral cortex that terminates on lower motor neurons and interneurons in the spinal cord, controlling movements of the limbs and trunk. There are more than one million neur ...
. It is often found that impairments following stroke are either caused by damage to the same or adjacent neurological structures. A combination of these impairments is more likely than just one in isolation. Damage to the corticospinal
The pyramidal tracts include both the corticobulbar tract and the corticospinal tract. These are aggregations of efferent nerve fibers from the upper motor neurons that travel from the cerebral cortex and terminate either in the brainstem (''co ...
system results in an inability to activate muscles with enough force or in a coordinated manner, which can lead to paresis, loss of fractional movement, and abnormal muscle tone. Damage to the somatosensory cortical areas causes loss of somatosensation which results in an impaired ability to monitor movement.
Considering monoplegia as it relates to cerebral palsy, in premature infants, the most common cause of cerebral palsy is periventricular hemorrhagic
Bleeding, hemorrhage, haemorrhage or blood loss, is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vag ...
infarction
Infarction is tissue death (necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct
(from the ...
. In term infants, the underlying causes are often cerebral malformations, cerebral infarction
Infarction is tissue death (necrosis) due to inadequate blood supply to the affected area. It may be caused by artery blockages, rupture, mechanical compression, or vasoconstriction. The resulting lesion is referred to as an infarct
(from the ...
, and intracerebral hemorrhage
Intracerebral hemorrhage (ICH), also known as cerebral bleed, intraparenchymal bleed, and hemorrhagic stroke, or haemorrhagic stroke, is a sudden bleeding into Intraparenchymal hemorrhage, the tissues of the brain, into its Intraventricular hemor ...
. Delayed crawling or walking are the usual concerns that arise in infants with paralysis of the limb. In these cases, abnormalities of the legs are the main focus of the attention.
Diagnosis
Monoplegia is diagnosed by a physician after a physical examination and sometimes after further neurologic examination as well. As monoplegia is fairly rare, after physical examination of a patient complaining of monoplegia, sometimes weakness of an additional limb is also identified and the patient is diagnosed withhemiplegia
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body ('' hemi-'' means "half"). Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medic ...
or paraplegia
Paraplegia, or paraparesis, is an impairment in motor or sensory function of the lower extremities. The word comes from Ionic Greek ()
"half-stricken". It is usually caused by spinal cord injury or a congenital condition that affects the neural ...
instead. After neurologic examination of the limb, a diagnosis of a monoplegic limb can be given if the patient receives a Medical Research Council power grade of 0, which is a measurement of the patient's limb strength. Needle Electromyography is often used to study all limbs, essentially showing the extent in each limb involvement. Furthermore, magnetic resonance imaging
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio wave ...
(MRI) is the diagnostic modality of choice for investigating all forms of hemiplegia. It is especially informative to show migrational defects in hemiplegic cerebral palsy associated with seizures.
An approach called single-pulse transcranial magnetic stimulation
Transcranial magnetic stimulation (TMS) is a noninvasive form of brain stimulation in which a changing magnetic field is used to induce an electric current at a specific area of the brain through electromagnetic induction. An electric pulse gener ...
(spTMS) has also been used to help diagnose motor deficits such as monoplegia. This is done by evaluating the functional level of the corticospinal tract through stimulation of the corticospinal lesions in order to obtain neurophysiologic evidence on the integrity of the corticospinal tracts. Single-pulse transcranial magnetic stimulation
Transcranial magnetic stimulation (TMS) is a noninvasive form of brain stimulation in which a changing magnetic field is used to induce an electric current at a specific area of the brain through electromagnetic induction. An electric pulse gener ...
provides neuropsychological feedback such as motor-evoked potentials (MEPs) and central motor conduction time (CMCT). This feedback can then be compared to the normal limits of patients who do not show evidence of deficits in the corticospinal tracts.
Treatment
There is no cure for monoplegia, but treatments typically include physical therapy and counseling to help recover muscle tone and function. Recovery will vary depending on diagnosis of temporary, partial or complete paralysis. Much of the therapies focus on the upper limb due to the fact that monoplegia in the upper limbs is much more common than in the lower limbs. It has been found that intense activity-based and goal-directed therapy, such asconstraint-induced movement therapy
Constraint-induced movement therapy (CI, CIT, or CIMT) is a form of rehabilitation therapy that improves upper extremity function in stroke and other central nervous system damage patients by increasing the use of their affected upper limb.
and bimanual therapy, are more effective than standard care. Studies suggest the less affected hand could provide a template for improving motor performance of the more affected hand, and provides a strong rationale for the development of bimanual training approaches. In addition to that, there is strong evidence to support that occupational therapy home programs that are goal-directed could be used to supplement hands-on direct therapy.
Constraint-induced movement therapy (CIMT) is specifically targeted at upper limb monoplegia as a result of a stroke. In CIMT the unaffected arm is restrained, forcing the use and frequent practice of the affected arm. This approach to therapy is carried out during ordinary and daily activities by the affected person. It has been found that CIMT is more effective at specifically improving arm movement than a physiotherapy
Physical therapy (PT), also known as physiotherapy, is one of the allied health professions. It is provided by physical therapists who promote, maintain, or restore health through physical examination, diagnosis, management, prognosis, patient ...
approach or no treatment at all. This type of therapy has proved to provide an only moderate improvement in patients with monoplegia. More research needs to be conducted in order to establish the lasting benefit of constraint-induced movement therapy.
Brain computer interface (BCI) systems have been proposed as a tool for rehabilitation of monoplegia, specifically in the upper limb after a stroke. BCI systems provide sensory feedback in the brain via functional electrical stimulation, virtual reality
Virtual reality (VR) is a simulated experience that employs pose tracking and 3D near-eye displays to give the user an immersive feel of a virtual world. Applications of virtual reality include entertainment (particularly video games), educ ...
environments, or robotic systems, which allows for the use of brain signals. This is extremely crucial because the networking in the brain is often compromised after a stroke, leading to impaired movement or paralysis. BCI systems allow for detection of intention to move through the primary motor cortex, then provide the matched sensory stimulation
In physiology, a stimulus is a detectable change in the physical or chemical structure of an organism's internal or external environment. The ability of an organism or organ to detect external stimuli, so that an appropriate reaction can be m ...
according to feedback that is provided. This leads to activity-dependent plasticity Activity-dependent plasticity is a form of functional and structural neuroplasticity that arises from the use of cognitive functions and personal experience; hence, it is the biological basis for learning and the formation of new memories. Activity- ...
within the user, requiring them to pay careful attention to tasks that require the activation or deactivation of specific brain areas. BCI systems utilize different sources of information for feedback, including electroencephalography
Electroencephalography (EEG) is a method to record an electrogram of the spontaneous electrical activity of the brain. The biosignals detected by EEG have been shown to represent the postsynaptic potentials of pyramidal neurons in the neocortex ...
(EEG), magnetoencephalography
Magnetoencephalography (MEG) is a functional neuroimaging technique for mapping brain activity by recording magnetic fields produced by electrical currents occurring naturally in the brain, using very sensitive magnetometers. Arrays of SQUIDs (su ...
, functional magnetic resonance imaging
Functional magnetic resonance imaging or functional MRI (fMRI) measures brain activity by detecting changes associated with blood flow. This technique relies on the fact that cerebral blood flow and neuronal activation are coupled. When an area o ...
, near-infrared spectroscopy
Near-infrared spectroscopy (NIRS) is a spectroscopic method that uses the near-infrared region of the electromagnetic spectrum (from 780 nm to 2500 nm). Typical applications include medical and physiological diagnostics and research incl ...
, or electrocorticography
Electrocorticography (ECoG), or intracranial electroencephalography (iEEG), is a type of electrophysiological monitoring that uses electrodes placed directly on the exposed surface of the brain to record electrical activity from the cerebral co ...
. Among all of these, the EEG signals are the most useful for this type of rehabilitation because they are highly accurate and stable.
Another form of treatment for monoplegia is functional electrical stimulation
Functional electrical stimulation (FES) is a technique that uses low-energy electrical pulses to artificially generate body movements in individuals who have been paralyzed due to injury to the central nervous system. More specifically, FES can ...
(FES). It is targeted at patients who acquired monoplegia through incidents such as a spinal cord injury
A spinal cord injury (SCI) is damage to the spinal cord that causes temporary or permanent changes in its function. Symptoms may include loss of muscle function, sensation, or autonomic function in the parts of the body served by the spinal cor ...
, stroke, multiple sclerosis
Multiple (cerebral) sclerosis (MS), also known as encephalomyelitis disseminata or disseminated sclerosis, is the most common demyelinating disease, in which the insulating covers of nerve cells in the brain and spinal cord are damaged. This d ...
, or cerebral palsy and utilizes electrical stimulation in order to cause the remaining motor units in the paralyzed muscles to contract. As in traditional muscular training, FES improves the force with which the unaffected muscles contract. For less severely affected patients, FES allows for greater improvement in range of motion than traditional physical therapy.
References
External links
{{Movement and gait symptoms and signs Symptoms and signs