Medical Deserts In The United States on:
[Wikipedia]
[Google]
[Amazon]
The  Proposed solutions to US health care deserts include the enactment of a national
Proposed solutions to US health care deserts include the enactment of a national
 About 20% of Americans live in rural regions, but only nine percent of the country's doctors practice in rural areas. Federal health officials predicted in 2019 that the number of rural doctors, half of them over 50 years of age, would decline by 23 percent during the next ten years. A contributing factor to this decline is newly graduated doctors' reluctance to move to rural areas. While doctors originally from rural areas are more likely to return to rural areas to practice, rural Americans are less likely to attend medical school in the first place. Newly graduated doctors have also tended to prefer jobs in hospitals, rather than jobs in family practices that are more common in rural areas.
Only 1% of medical students in their final year of school prefer to live in communities under 10,000. The lack of entertainment or food diversity, fear of prejudice, and reduced financial prospects associated with rural regions have been cited as factors leading to medical students' reluctance to practice in rural regions, as well as the unique difficulties associated with practice rural healthcare. For example, in parts of rural Alaska, transferring patients to hospital emergency rooms can "depend on the schedules of rickety charter planes" which are often prevented from flying due to the weather. In some states, such as Oklahoma, a lack of available residency programs for prospective doctors directly contributes to a shortage.
About 20% of Americans live in rural regions, but only nine percent of the country's doctors practice in rural areas. Federal health officials predicted in 2019 that the number of rural doctors, half of them over 50 years of age, would decline by 23 percent during the next ten years. A contributing factor to this decline is newly graduated doctors' reluctance to move to rural areas. While doctors originally from rural areas are more likely to return to rural areas to practice, rural Americans are less likely to attend medical school in the first place. Newly graduated doctors have also tended to prefer jobs in hospitals, rather than jobs in family practices that are more common in rural areas.
Only 1% of medical students in their final year of school prefer to live in communities under 10,000. The lack of entertainment or food diversity, fear of prejudice, and reduced financial prospects associated with rural regions have been cited as factors leading to medical students' reluctance to practice in rural regions, as well as the unique difficulties associated with practice rural healthcare. For example, in parts of rural Alaska, transferring patients to hospital emergency rooms can "depend on the schedules of rickety charter planes" which are often prevented from flying due to the weather. In some states, such as Oklahoma, a lack of available residency programs for prospective doctors directly contributes to a shortage.
 The federal government is legally obligated under treaties to provide medical care to
The federal government is legally obligated under treaties to provide medical care to
 A team of researchers found that in Los Angeles 89 percent of Black-majority census tracts were situated in trauma deserts; in Chicago, 73 percent; in New York City 14 percent. In Los Angeles County, South Los Angeles with one-million residents and the highest mortality rate in the county, also has the highest rates of disease and premature deaths from preventable conditions: "coronary heart disease, homicide, diabetes, lung cancer, and motor vehicle crashes." In economically stressed South LA, there are 11 pediatricians for every 100,000 children, whereas in upscale West Los Angeles there are almost 200 pediatricians for every100,000 children. In West LA, 12 percent of adults are uninsured compared to 30 percent in South LA.
Even as health care delivery models shift from hospitals to community clinics offering Urgent Care in once-vacant retail spaces, poor neighborhoods face inequities with the distribution of community clinics in predominantly wealthier suburban neighborhoods.
A team of researchers found that in Los Angeles 89 percent of Black-majority census tracts were situated in trauma deserts; in Chicago, 73 percent; in New York City 14 percent. In Los Angeles County, South Los Angeles with one-million residents and the highest mortality rate in the county, also has the highest rates of disease and premature deaths from preventable conditions: "coronary heart disease, homicide, diabetes, lung cancer, and motor vehicle crashes." In economically stressed South LA, there are 11 pediatricians for every 100,000 children, whereas in upscale West Los Angeles there are almost 200 pediatricians for every100,000 children. In West LA, 12 percent of adults are uninsured compared to 30 percent in South LA.
Even as health care delivery models shift from hospitals to community clinics offering Urgent Care in once-vacant retail spaces, poor neighborhoods face inequities with the distribution of community clinics in predominantly wealthier suburban neighborhoods.
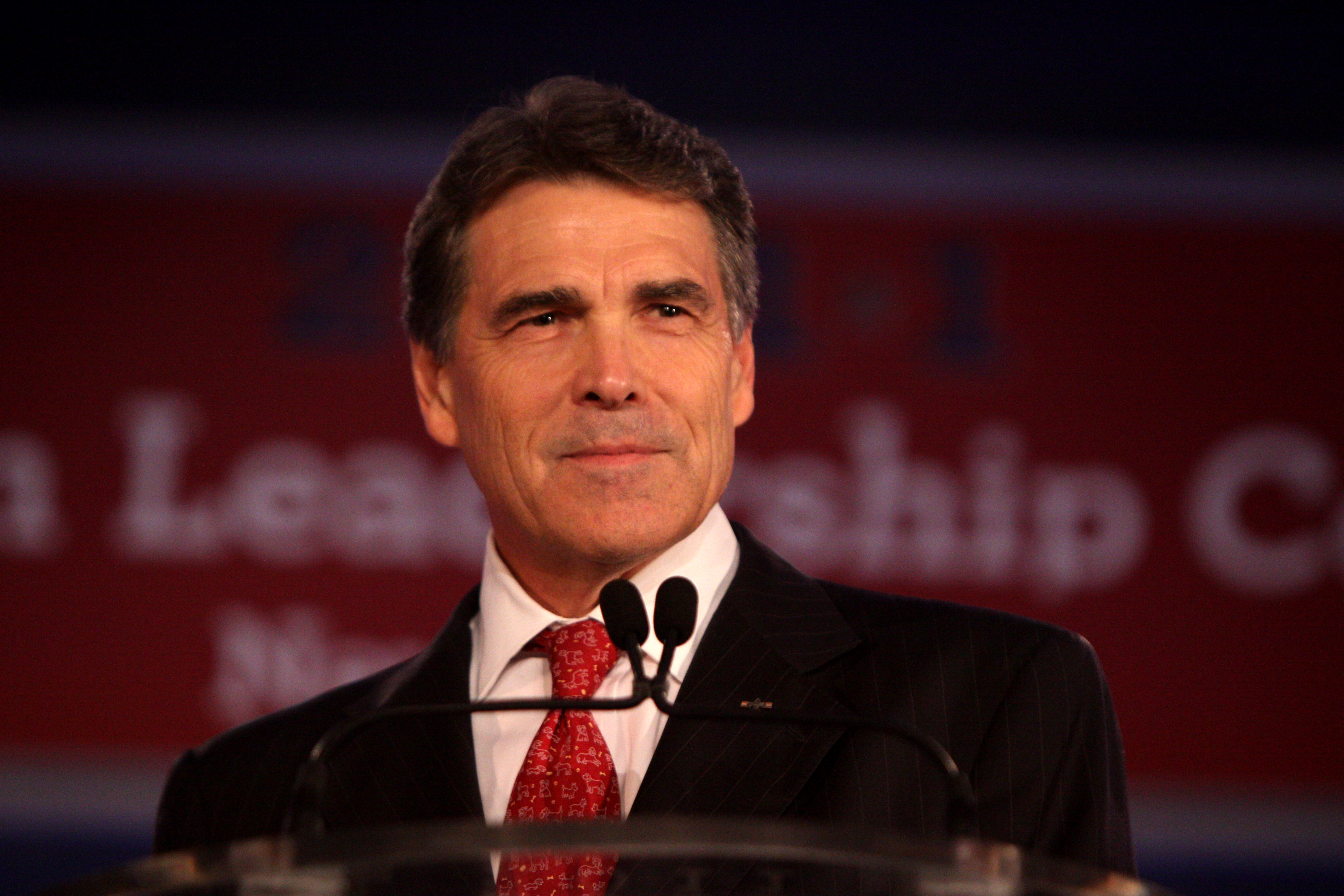 The 2010 passage of the Affordable Care Act expanded Medicaid eligibility for low income Americans, but several Southern states with large poor black populations opted out of the expansion, its Republican governors opposing the Obama-led initiative as federal over-reach. In rejecting Medicaid expansion—estimated at $100 billion federal dollars over 10 years—then Texas Governor Rick Perry told Tea Party supporters in 2013, "Texas will not be held hostage by the Obama administration's attempt to force us into this fool's errand of adding more than a million Texans to a broken system."
The 2010 passage of the Affordable Care Act expanded Medicaid eligibility for low income Americans, but several Southern states with large poor black populations opted out of the expansion, its Republican governors opposing the Obama-led initiative as federal over-reach. In rejecting Medicaid expansion—estimated at $100 billion federal dollars over 10 years—then Texas Governor Rick Perry told Tea Party supporters in 2013, "Texas will not be held hostage by the Obama administration's attempt to force us into this fool's errand of adding more than a million Texans to a broken system."
 Proponents of a national health insurance program to replace for-profit health insurance argue adoption of a federally funded single-payer system allowing patients to choose their own doctor would reduce "structural racism" in health care that results in non-white Americans suffering higher mortality rates in underserved communities. Backers of single-payer or Medicare for All note that minorities and the poor, as well as rural residents, in general, are less able to afford private health insurance, and that those who can must pay high deductibles and co-payments that threaten families with financial ruin. In addition, they argue that those with employment-based insurance are tethered to jobs for fear of losing their medical coverage while rural communities with high unemployment lose out on job-based insurance benefits.
Critics of Medicare for All oppose a government funded health care system, wanting to preserve a for-profit model to increase competition, and assert that hospitals, already financially vulnerable in rural America, would lose more money and risk bankruptcy because private insurance, on which they rely for financial stability, reimburses at higher rates than Medicare. Proponents argue, however, that proposed single-payer legislation in the House and Senate would boost hospital reimbursements far beyond current levels, while establishing annual global hospital funds that could be increased to cover unexpected costs and grant applications for capital improvements. Supporters of single-payer point to the closure of over 100 rural hospitals since 2010, with over 400 also at risk of closure, as evidence of the failure of a for-profit health insurance system unaffordable to many rural residents and unsustainable for hospitals that rely on reimbursements from private insurance.
Proponents of a national health insurance program to replace for-profit health insurance argue adoption of a federally funded single-payer system allowing patients to choose their own doctor would reduce "structural racism" in health care that results in non-white Americans suffering higher mortality rates in underserved communities. Backers of single-payer or Medicare for All note that minorities and the poor, as well as rural residents, in general, are less able to afford private health insurance, and that those who can must pay high deductibles and co-payments that threaten families with financial ruin. In addition, they argue that those with employment-based insurance are tethered to jobs for fear of losing their medical coverage while rural communities with high unemployment lose out on job-based insurance benefits.
Critics of Medicare for All oppose a government funded health care system, wanting to preserve a for-profit model to increase competition, and assert that hospitals, already financially vulnerable in rural America, would lose more money and risk bankruptcy because private insurance, on which they rely for financial stability, reimburses at higher rates than Medicare. Proponents argue, however, that proposed single-payer legislation in the House and Senate would boost hospital reimbursements far beyond current levels, while establishing annual global hospital funds that could be increased to cover unexpected costs and grant applications for capital improvements. Supporters of single-payer point to the closure of over 100 rural hospitals since 2010, with over 400 also at risk of closure, as evidence of the failure of a for-profit health insurance system unaffordable to many rural residents and unsustainable for hospitals that rely on reimbursements from private insurance.
 Proponents of a public option support expanding the Affordable Care Act to give consumers a choice; private for-profit health insurance or Medicare. Backers of the public option say the ACA has not gone far enough, noting that despite the United States spending a greater percentage of its GDP on health care than any other nation, there are still over 28-million people without health insurance, resulting in Americans in underserved communities dying for lack of affordable care or declaring bankruptcy because of mounting medical bills.
While advocates of a public option agree with single-payer proponents that the United States should provide universal health care, they disagree on the solution, asserting that Americans are not interested in a government-run health care system and want to be able to keep their private health insurance. Critics who support single-payer instead charge that offering a public option to compete with private insurance would create a two-tiered system of concierge versus minimal medical services, as private for-profit insurance companies use political muscle to deny coverage to the oldest and sickest Americans, thus shunting the more expensive patients onto a financially vulnerable public option. Medicare for All proponents also say a hybrid system of private insurance coupled with a public option would result in added bureaucracy and paperwork, and therefore fail to lower health care costs.
Those favoring a strictly for-profit health care model claim a public option, with lower hospital reimbursements than private insurance, would bankrupt rural hospitals dependent on higher reimbursements from commercial insurance vendors.
Proponents of a public option support expanding the Affordable Care Act to give consumers a choice; private for-profit health insurance or Medicare. Backers of the public option say the ACA has not gone far enough, noting that despite the United States spending a greater percentage of its GDP on health care than any other nation, there are still over 28-million people without health insurance, resulting in Americans in underserved communities dying for lack of affordable care or declaring bankruptcy because of mounting medical bills.
While advocates of a public option agree with single-payer proponents that the United States should provide universal health care, they disagree on the solution, asserting that Americans are not interested in a government-run health care system and want to be able to keep their private health insurance. Critics who support single-payer instead charge that offering a public option to compete with private insurance would create a two-tiered system of concierge versus minimal medical services, as private for-profit insurance companies use political muscle to deny coverage to the oldest and sickest Americans, thus shunting the more expensive patients onto a financially vulnerable public option. Medicare for All proponents also say a hybrid system of private insurance coupled with a public option would result in added bureaucracy and paperwork, and therefore fail to lower health care costs.
Those favoring a strictly for-profit health care model claim a public option, with lower hospital reimbursements than private insurance, would bankrupt rural hospitals dependent on higher reimbursements from commercial insurance vendors.
United States
The United States of America (U.S.A. or USA), commonly known as the United States (U.S. or US) or America, is a country primarily located in North America. It consists of 50 states, a federal district, five major unincorporated territorie ...
has many regions which have been described as medical desert
Medical desert is a term used to describe regions whose population has inadequate access to healthcare. The term can be applied whether the lack of healthcare is general or in a specific field, such as dental or pharmaceutical. It is primarily used ...
s, with those locations featuring inadequate access to one or more kinds of medical services. An estimated thirty million Americans, many in rural regions of the country, live at least a sixty minute drive from a hospital
A hospital is a health care institution providing patient treatment with specialized health science and auxiliary healthcare staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emerge ...
with trauma care services. Limited access to emergency room services, as well as medical specialists, leads to increases in mortality rate
Mortality rate, or death rate, is a measure of the number of deaths (in general, or due to a specific cause) in a particular population, scaled to the size of that population, per unit of time. Mortality rate is typically expressed in units of de ...
s and long-term health problems, such as heart disease
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, hea ...
and diabetes
Diabetes, also known as diabetes mellitus, is a group of metabolic disorders characterized by a high blood sugar level ( hyperglycemia) over a prolonged period of time. Symptoms often include frequent urination, increased thirst and increased ap ...
. Regions with higher rates of Medicaid and Medicare patients, as well patients who are uninsured are less likely to live within an hour's drive of a hospital emergency room.
Since 1975, over 1,000 hospitals, many in rural regions, have closed their doors, unable to bear the cost of care of uninsured patients, resulting in some patients in every state needing to drive at least an hour to a hospital emergency room, a problem that poses an even greater danger during the COVID-19 pandemic
The COVID-19 pandemic, also known as the coronavirus pandemic, is an ongoing global pandemic of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The novel virus was first identif ...
, when patients in respiratory distress
Shortness of breath (SOB), also medically known as dyspnea (in AmE) or dyspnoea (in BrE), is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing disc ...
urgently need oxygen and can ill afford an hour-long ambulance ride to reach a hospital. In addition to the immediate financial problems facing rural healthcare providers, inequities in rural healthcare are further aggravated by the disproportionately low amount of newly graduated doctors that apply for positions in rural areas.
Although concentrated in rural regions, health care deserts also exist in urban and suburban areas, particularly in Black
Black is a color which results from the absence or complete absorption of visible light. It is an achromatic color, without hue, like white and grey. It is often used symbolically or figuratively to represent darkness. Black and white have o ...
majority census tracts in Chicago
(''City in a Garden''); I Will
, image_map =
, map_caption = Interactive Map of Chicago
, coordinates =
, coordinates_footnotes =
, subdivision_type = Country
, subdivision_name ...
, Los Angeles
Los Angeles ( ; es, Los Ángeles, link=no , ), often referred to by its initials L.A., is the largest city in the state of California and the second most populous city in the United States after New York City, as well as one of the world' ...
and New York City
New York, often called New York City or NYC, is the List of United States cities by population, most populous city in the United States. With a 2020 population of 8,804,190 distributed over , New York City is also the L ...
. Medical literature addressing health disparities in urban centers has applied the term medical desert to areas that are more than a five-miles from the nearest acute care
Acute care is a branch of secondary health care where a patient receives active but short-term treatment for a severe injury or episode of illness, an urgent medical condition, or during recovery from surgery.Alberta Health ServicesAcute care.Acces ...
facility. Racial demographic disparities in healthcare access are also present in rural areas, with Native Americans living in rural areas in particular receiving inadequate medical care. Proposed solutions to US health care deserts include the enactment of a national
Proposed solutions to US health care deserts include the enactment of a national single payer health care
Single-payer healthcare is a type of universal healthcare in which the costs of essential healthcare for all residents are covered by a single public system (hence "single-payer").
Single-payer systems may contract for healthcare services from ...
system; adoption of a public option
The public health insurance option, also known as the public insurance option or the public option, is a proposal to create a government-run health insurance agency that would compete with other private health insurance companies within the United ...
under the Affordable Care Act
The Affordable Care Act (ACA), formally known as the Patient Protection and Affordable Care Act and colloquially known as Obamacare, is a landmark U.S. federal statute enacted by the 111th United States Congress and signed into law by Presid ...
(ACA); the approval of higher Medicare reimbursements and tax credits for struggling hospitals; the establishment of strategically placed free-standing emergency centers; the expansion of telehealth
Telehealth is the distribution of health-related services and information via electronic information and telecommunication technologies. It allows long-distance patient and clinician contact, care, advice, reminders, education, intervention, mon ...
and telemedicine to remote areas; and increased incentives to recruit doctors to practice in rural and underserved areas.
In December 2021, an article from the financial publication ''Forbes
''Forbes'' () is an American business magazine owned by Integrated Whale Media Investments and the Forbes family. Published eight times a year, it features articles on finance, industry, investing, and marketing topics. ''Forbes'' also re ...
'' argued that the "lack of funding for residency slots to expand the pool of physicians in the U.S. has been an issue for more than two decades." Other American news agencies such as ''The Nation
''The Nation'' is an American liberal biweekly magazine that covers political and cultural news, opinion, and analysis. It was founded on July 6, 1865, as a successor to William Lloyd Garrison's '' The Liberator'', an abolitionist newspaper tha ...
'' and ''Newsweek
''Newsweek'' is an American weekly online news magazine co-owned 50 percent each by Dev Pragad, its president and CEO, and Johnathan Davis (businessman), Johnathan Davis, who has no operational role at ''Newsweek''. Founded as a weekly print m ...
'' have additionally addressed the topic. Addressing the doctor shortage in the U.S. remains a challenge in terms of improving healthcare in America. In the 2010s, a study released by the Association of American Medical Colleges (AAMC) titled ''The Complexities of Physician Supply and Demand: Projections From 2019 to 2034'' specifically projected a shortage of between 37,800 and 124,000 individuals within the following two decades, approximately.
In rural areas
In 2019, thefederal government
A federation (also known as a federal state) is a political entity characterized by a union of partially self-governing provinces, states, or other regions under a central federal government (federalism). In a federation, the self-governin ...
identified nearly 80 percent of rural America as “medically underserved,” lacking in skilled nursing facilities, as well as rehabilitation
Rehabilitation or Rehab may refer to:
Health
* Rehabilitation (neuropsychology), therapy to regain or improve neurocognitive function that has been lost or diminished
* Rehabilitation (wildlife), treatment of injured wildlife so they can be retur ...
, psychiatric and intensive care units. In rural areas, there are approximately 68 primary care doctors per 100,000 people, whereas there are 84 doctors per 100,000 in urban centers. According to the National Rural Health Association
The National Rural Health Association (NRHA) is a national nonprofit professional association in the United States with more than 18,000 members. The association’s mission is to provide leadership on rural health issues, which it attempts to carr ...
, 9% of rural counties had no doctors in 2017. Rural communities face lower life expectancy and increased rates of diabetes, chronic disease, and obesity. Fewer than half of rural women live within a thirty-minute drive of the nearest hospital able to provide obstetric services, and 12% do not live within a sixty-minute drive of the nearest such hospital, resulting in babies sometimes being born on the side of the road and increased maternal and infant mortality rates.
Rural residents may live on farms, ranches and Indian reservations far from a hospital, forcing residents to take several hours or an entire day off work to drive to a doctor's appointment or follow up care, making rural residents less likely to seek treatment. The Centers for Disease Control and Prevention
The Centers for Disease Control and Prevention (CDC) is the national public health agency of the United States. It is a United States federal agency, under the Department of Health and Human Services, and is headquartered in Atlanta, Georgi ...
(CDC) reports that during 1999–2014 rural counties experienced increased mortality rates from the five leading causes of death (1-heart disease, 2-cancer, 3-unintentional injury, 4-chronic lower respiratory disease (CLRD), 5-stroke) compared with metropolitan counties. For unintentional injuries (high speed car accidents; opioid and drug abuse and traumatic brain injuries) mortality rates were approximately 50% higher in rural areas than urban areas", with inadequate access to adequately staffed healthcare facilities listed as one among several factors leading to this disparity.
In states that chose not to expand Medicaid programs under the Affordable Care Act–Alabama
(We dare defend our rights)
, anthem = "Alabama (state song), Alabama"
, image_map = Alabama in United States.svg
, seat = Montgomery, Alabama, Montgomery
, LargestCity = Huntsville, Alabama, Huntsville
, LargestCounty = Baldwin County, Al ...
, Georgia, Missouri
Missouri is a U.S. state, state in the Midwestern United States, Midwestern region of the United States. Ranking List of U.S. states and territories by area, 21st in land area, it is bordered by eight states (tied for the most with Tennessee ...
, Oklahoma
Oklahoma (; Choctaw language, Choctaw: ; chr, ᎣᎧᎳᎰᎹ, ''Okalahoma'' ) is a U.S. state, state in the South Central United States, South Central region of the United States, bordered by Texas on the south and west, Kansas on the nor ...
, Texas
Texas (, ; Spanish language, Spanish: ''Texas'', ''Tejas'') is a state in the South Central United States, South Central region of the United States. At 268,596 square miles (695,662 km2), and with more than 29.1 million residents in 2 ...
and Tennessee
Tennessee ( , ), officially the State of Tennessee, is a landlocked state in the Southeastern region of the United States. Tennessee is the 36th-largest by area and the 15th-most populous of the 50 states. It is bordered by Kentucky to th ...
–rural Americans face limited options as hospitals close their doors. A 2019 study found that participation in Medicaid expansion reduced the likelihood of rural hospital closures by 62% and that of the hospitals deemed most at-risk for closure, 75% were in states that did not expand Medicare.
In 2016, the Kaiser Commission on Medicaid and the Uninsured, in conjunction with the Urban Institute, conducted a case study analysis of three privately owned Southern hospitals to determine the causes and effects of their closures in Kansas
Kansas () is a state in the Midwestern United States. Its capital is Topeka, and its largest city is Wichita. Kansas is a landlocked state bordered by Nebraska to the north; Missouri to the east; Oklahoma to the south; and Colorado to the ...
, Kentucky
Kentucky ( , ), officially the Commonwealth of Kentucky, is a state in the Southeastern region of the United States and one of the states of the Upper South. It borders Illinois, Indiana, and Ohio to the north; West Virginia and Virginia to ...
and South Carolina
)''Animis opibusque parati'' ( for, , Latin, Prepared in mind and resources, links=no)
, anthem = " Carolina";" South Carolina On My Mind"
, Former = Province of South Carolina
, seat = Columbia
, LargestCity = Charleston
, LargestMetro = ...
. In addition to the challenges of graying, declining and poverty-stricken populations, as well as the preference of privately insured patients to seek treatment at newer hospitals further away, the report said corporate profit-driven decisions, as opposed to local community needs, shuttered the doors of rural hospitals in underserved areas. In a "shift from mission to margin," health systems that owned multiple hospitals, some more profitable than others, closed less-profitable hospitals in Kentucky and South Carolina to concentrate resources on other hospitals in the chain, resulting in communities without acute care and emergency facilities to serve as a safety-net for patients facing challenges with mental health and drug use. The case studies report also notes that decreases in Medicare and Medicaid reimbursements, some the result of federal budget sequestration or across the board cuts, others the result of the Affordable Care Act's lower hospital Medicare readmission reimbursement rates, negatively impacted the finances of the rural hospitals.
Physician shortages
 About 20% of Americans live in rural regions, but only nine percent of the country's doctors practice in rural areas. Federal health officials predicted in 2019 that the number of rural doctors, half of them over 50 years of age, would decline by 23 percent during the next ten years. A contributing factor to this decline is newly graduated doctors' reluctance to move to rural areas. While doctors originally from rural areas are more likely to return to rural areas to practice, rural Americans are less likely to attend medical school in the first place. Newly graduated doctors have also tended to prefer jobs in hospitals, rather than jobs in family practices that are more common in rural areas.
Only 1% of medical students in their final year of school prefer to live in communities under 10,000. The lack of entertainment or food diversity, fear of prejudice, and reduced financial prospects associated with rural regions have been cited as factors leading to medical students' reluctance to practice in rural regions, as well as the unique difficulties associated with practice rural healthcare. For example, in parts of rural Alaska, transferring patients to hospital emergency rooms can "depend on the schedules of rickety charter planes" which are often prevented from flying due to the weather. In some states, such as Oklahoma, a lack of available residency programs for prospective doctors directly contributes to a shortage.
About 20% of Americans live in rural regions, but only nine percent of the country's doctors practice in rural areas. Federal health officials predicted in 2019 that the number of rural doctors, half of them over 50 years of age, would decline by 23 percent during the next ten years. A contributing factor to this decline is newly graduated doctors' reluctance to move to rural areas. While doctors originally from rural areas are more likely to return to rural areas to practice, rural Americans are less likely to attend medical school in the first place. Newly graduated doctors have also tended to prefer jobs in hospitals, rather than jobs in family practices that are more common in rural areas.
Only 1% of medical students in their final year of school prefer to live in communities under 10,000. The lack of entertainment or food diversity, fear of prejudice, and reduced financial prospects associated with rural regions have been cited as factors leading to medical students' reluctance to practice in rural regions, as well as the unique difficulties associated with practice rural healthcare. For example, in parts of rural Alaska, transferring patients to hospital emergency rooms can "depend on the schedules of rickety charter planes" which are often prevented from flying due to the weather. In some states, such as Oklahoma, a lack of available residency programs for prospective doctors directly contributes to a shortage.
Impact on Native Americans and Alaskan Natives
 The federal government is legally obligated under treaties to provide medical care to
The federal government is legally obligated under treaties to provide medical care to American Indian and Alaska Native
Native Americans, also known as American Indians, First Americans, Indigenous Americans, and #Terminology differences, other terms, are the Indigenous peoples of the Americas, Indigenous peoples of the mainland United States (Indigenous peopl ...
Americans through the Indian Health Service (IHS), part of the United States Department of Health and Human Services
The United States Department of Health and Human Services (HHS) is a cabinet-level executive branch department of the U.S. federal government created to protect the health of all Americans and providing essential human services. Its motto is ...
. Advocates for the Native American community have argued, however, that the government chronically under funds the IHS, resulting in a lack of accessible health care facilities, particularly emergency room departments for those living on reservations. The IHS provides services to 573 tribes and 2.56 million Native Americans primarily living on or near reservations and in rural areas concentrated in Alaska and the western United States. In 2011, the IHS reported that life expectancy for Native Americans was 73, compared to 78 for all other races in the US, as Native Americans and Alaskan natives were dying at higher rates due to chronic liver disease, diabetes, intentional self-harm and suicide, as well as respiratory diseases. In 2016, the Office of Inspector General
In the United States, Office of Inspector General (OIG) is a generic term for the oversight division of a federal or state agency aimed at preventing inefficient or unlawful operations within their parent agency. Such offices are attached to man ...
(OIG) issued reports criticizing the IHS's hospital care for tribal members, citing lack of oversight, outdated equipment and difficulty in recruiting and retaining skilled staff. Administrators at one hospital interviewed by the OIG complained of aging hospital infrastructure with corroded pipes causing sewage to spill into an operating room.
Dissatisfied with the IHS's management of health clinics and hospitals closest to reservations, tribes
The term tribe is used in many different contexts to refer to a category of human social group. The predominant worldwide usage of the term in English is in the discipline of anthropology. This definition is contested, in part due to conflic ...
have demanded greater control over hospital administration. In July, 2019, the Great Plains Tribal Chairmen's Health Board representing 18 tribal communities in South Dakota
South Dakota (; Sioux language, Sioux: , ) is a U.S. state in the West North Central states, North Central region of the United States. It is also part of the Great Plains. South Dakota is named after the Lakota people, Lakota and Dakota peo ...
, North Dakota
North Dakota () is a U.S. state in the Upper Midwest, named after the Native Americans in the United States, indigenous Dakota people, Dakota Sioux. North Dakota is bordered by the Canadian provinces of Saskatchewan and Manitoba to the north a ...
, Nebraska
Nebraska () is a state in the Midwestern region of the United States. It is bordered by South Dakota to the north; Iowa to the east and Missouri to the southeast, both across the Missouri River; Kansas to the south; Colorado to the southwe ...
and Iowa
Iowa () is a state in the Midwestern region of the United States, bordered by the Mississippi River to the east and the Missouri River and Big Sioux River to the west. It is bordered by six states: Wisconsin to the northeast, Illinois to the ...
, took over the Rapid City's Sioux San Hospital
The Rapid City Indian Health Service Hospital formerly known as The Sioux San Hospital is an Indian Health Service hospital located in Rapid City, South Dakota. It was built in 1898 as a boarding school for Native Americans and turned into a sani ...
, where, according to government investigators, patients died as a result of misdiagnoses and treatment by staff members not screened for hepatitis and tuberculosis.
In New Mexico, where Native Americans, in 2020, make up six percent of the population but 25% of positive COVID-19 cases, members of the Navajo Nation live without access to running water to frequently wash their hands, as recommended by the CDC.
In urban areas
According to research conducted in 2019 by University of Chicago Medicine, African Americancensus tract
A census tract, census area, census district or meshblock is a geographic region defined for the purpose of taking a census. Sometimes these coincide with the limits of cities, towns or other administrative areas and several tracts commonly exist ...
s in large US cities—Chicago, Los Angeles, New York City—are more likely than white majority neighborhoods to be located in trauma care deserts that are greater than five miles from a trauma center offering emergency medical services and specialists: neurosurgeons, cardiac doctors, respiratory therapists.
 A team of researchers found that in Los Angeles 89 percent of Black-majority census tracts were situated in trauma deserts; in Chicago, 73 percent; in New York City 14 percent. In Los Angeles County, South Los Angeles with one-million residents and the highest mortality rate in the county, also has the highest rates of disease and premature deaths from preventable conditions: "coronary heart disease, homicide, diabetes, lung cancer, and motor vehicle crashes." In economically stressed South LA, there are 11 pediatricians for every 100,000 children, whereas in upscale West Los Angeles there are almost 200 pediatricians for every100,000 children. In West LA, 12 percent of adults are uninsured compared to 30 percent in South LA.
Even as health care delivery models shift from hospitals to community clinics offering Urgent Care in once-vacant retail spaces, poor neighborhoods face inequities with the distribution of community clinics in predominantly wealthier suburban neighborhoods.
A team of researchers found that in Los Angeles 89 percent of Black-majority census tracts were situated in trauma deserts; in Chicago, 73 percent; in New York City 14 percent. In Los Angeles County, South Los Angeles with one-million residents and the highest mortality rate in the county, also has the highest rates of disease and premature deaths from preventable conditions: "coronary heart disease, homicide, diabetes, lung cancer, and motor vehicle crashes." In economically stressed South LA, there are 11 pediatricians for every 100,000 children, whereas in upscale West Los Angeles there are almost 200 pediatricians for every100,000 children. In West LA, 12 percent of adults are uninsured compared to 30 percent in South LA.
Even as health care delivery models shift from hospitals to community clinics offering Urgent Care in once-vacant retail spaces, poor neighborhoods face inequities with the distribution of community clinics in predominantly wealthier suburban neighborhoods.
COVID-19 impacts on urban communities of color
African Americans account for a disproportionate number ofCOVID-19
Coronavirus disease 2019 (COVID-19) is a contagious disease caused by a virus, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first known case was COVID-19 pandemic in Hubei, identified in Wuhan, China, in December ...
fatalities due to multiple factors, including greater exposure in use of public transportation and employment in care-giving, sanitation and retail, underlying health conditions, as well as lack of access to nearby medical health clinics and hospitals and inadequate health insurance. In an April 2020 analysis of early data, the Washington Post found that counties with a majority of Black residents faced three times the rate of COVID-19 infections and almost six times the rate of deaths as majority white counties. The American Medical Association (AMA), noting structural inequities gripping communities of color, urged the federal government to collect COVID-19 data by race and ethnicity.
During the COVID-19 crisis, New York Times reporter Michael Schwirtz wrote (April 26, 2020) of the disparities in hospital services and finances between New York's white communities and those of color, with a private hospital closer to Wall Street able to tap reserves and exercise political influence to treat more patients, boost testing and obtain protective gear, even arrange for a plane from billionaire Warren Buffett's company to fly in masks from China, while a Brooklyn public hospital serving patients predominantly poor and of color resorts to plastic and duct tape to separate infectious patients' quarters and launches a Go Fund Me page to raise money for masks, gowns and booties to protect doctors and nurses from a virus that is "killing black and Latino New Yorkers at about twice the rate of white residents."
Racial disparities in health care
Scholars and researchers trace the roots of African American health care inequities tochattel slavery
Slavery and enslavement are both the state and the condition of being a slave—someone forbidden to quit one's service for an enslaver, and who is treated by the enslaver as property. Slavery typically involves slaves being made to perf ...
, Jim Crow laws
The Jim Crow laws were state and local laws enforcing racial segregation in the Southern United States. Other areas of the United States were affected by formal and informal policies of segregation as well, but many states outside the Sout ...
and institutional racism, with medical schools perpetuating stereotypes of racial inferiority up until the mid 20th century and scientists exploiting African Americans in unethical experimentation without informed consent. In The Atlantic's "Why American Health Care is still Segregated" (2016), reporter Vann Newkirk writes of Black Codes
The Black Codes, sometimes called the Black Laws, were laws which governed the conduct of African Americans (free and freed blacks). In 1832, James Kent (jurist), James Kent wrote that "in most of the United States, there is a distinction in re ...
that led to racially segregated clinics, doctors' offices and hospitals in which African Americans were assigned to separate wings to receive inferior medical treatment. In a 2008 address to the National Medical Association
The National Medical Association (NMA) is the largest and oldest national organization representing African American physicians and their patients in the United States. The NMA is a 501(c)(3) national professional and scientific organization repr ...
in 2008, Ronald M. Davis, MD, past president of the American Medical Association (AMA), apologized for the organization's history of excluding African-Americans from the AMA, pledging to "right the wrongs perpetrated against African American physicians, their families and patients."
Hundreds of years of geographical segregation left a legacy of segregated and understaffed hospitals serving African American communities. In a departure from the past, the National Association for the Advancement of Colored People
The National Association for the Advancement of Colored People (NAACP) is a civil rights organization in the United States, formed in 1909 as an interracial endeavor to advance justice for African Americans by a group including W. E. ...
(NAACP) in the 1960s won a US Supreme Court victory in Simkins v Moses H. Cone Memorial Hospital, a landmark ruling that barred the use of public funds to expand segregated hospitals. Still, racial segregation in the medical field persists, with African Americans living in black neighborhoods more likely than whites to undergo treatment at hospitals with higher surgical death rates, give birth at hospitals with higher neonatal mortality rates and live in nursing homes with fewer staff members and tenuous finances.
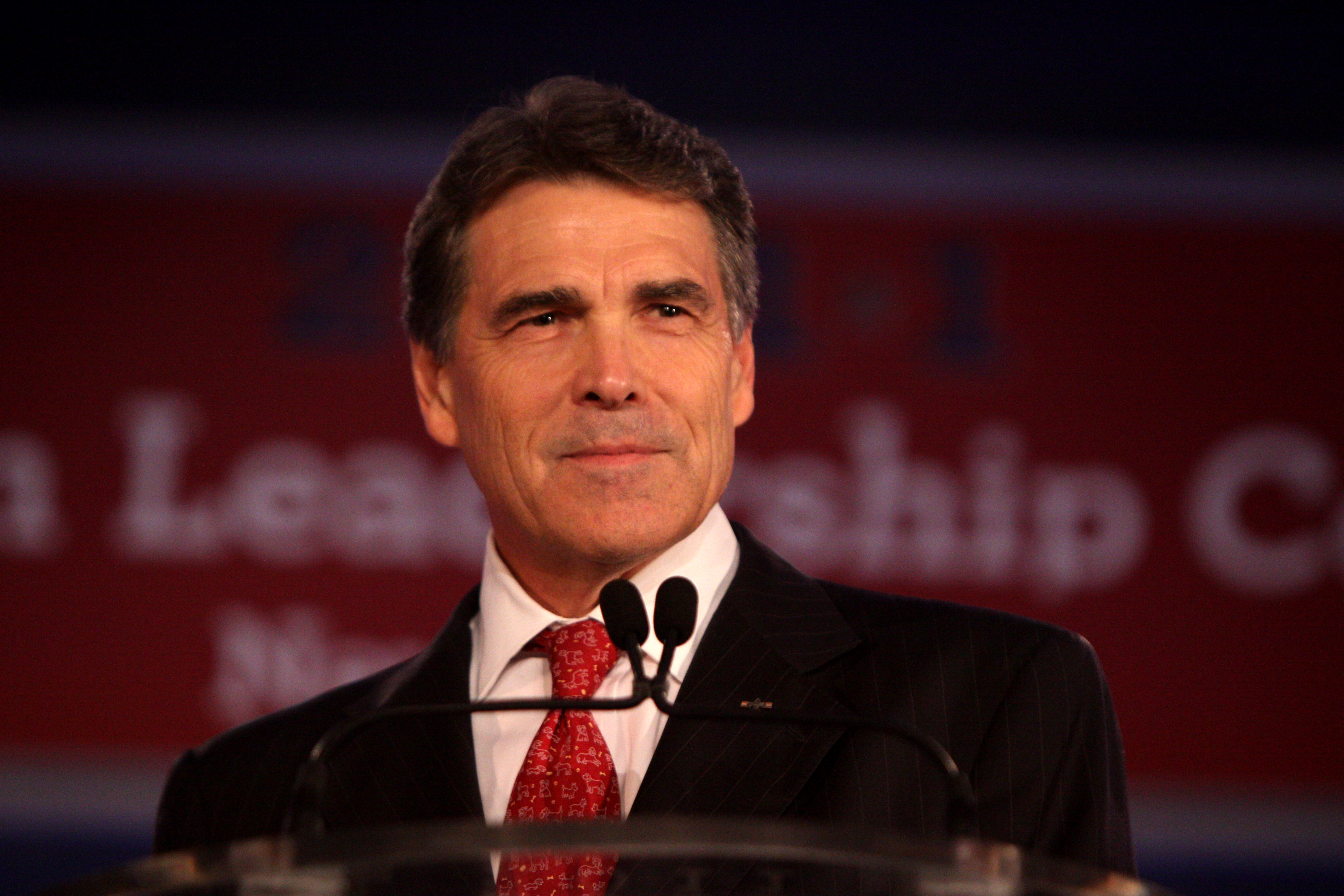 The 2010 passage of the Affordable Care Act expanded Medicaid eligibility for low income Americans, but several Southern states with large poor black populations opted out of the expansion, its Republican governors opposing the Obama-led initiative as federal over-reach. In rejecting Medicaid expansion—estimated at $100 billion federal dollars over 10 years—then Texas Governor Rick Perry told Tea Party supporters in 2013, "Texas will not be held hostage by the Obama administration's attempt to force us into this fool's errand of adding more than a million Texans to a broken system."
The 2010 passage of the Affordable Care Act expanded Medicaid eligibility for low income Americans, but several Southern states with large poor black populations opted out of the expansion, its Republican governors opposing the Obama-led initiative as federal over-reach. In rejecting Medicaid expansion—estimated at $100 billion federal dollars over 10 years—then Texas Governor Rick Perry told Tea Party supporters in 2013, "Texas will not be held hostage by the Obama administration's attempt to force us into this fool's errand of adding more than a million Texans to a broken system."
In suburban areas
Though suburbs often conjure images of affluence, a Health Affairs study using national survey data from 2005 to 2015 belies that picture. According to the survey, the suburbs, receiving a fraction of public health care funding compared to cities, are home to 17 million Americans who struggle in poverty, exceeding the numbers in urban centers and rural areas and straining hospitals with aging infrastructure. Additionally, the Health Affairs study noted large numbers of uninsured or Medicaid-reliant suburban dwellers either can't find doctors and hospitals who will serve them or must travel great distances to see specialists.Proposed solutions
Single-payer healthcare / Medicare for All
 Proponents of a national health insurance program to replace for-profit health insurance argue adoption of a federally funded single-payer system allowing patients to choose their own doctor would reduce "structural racism" in health care that results in non-white Americans suffering higher mortality rates in underserved communities. Backers of single-payer or Medicare for All note that minorities and the poor, as well as rural residents, in general, are less able to afford private health insurance, and that those who can must pay high deductibles and co-payments that threaten families with financial ruin. In addition, they argue that those with employment-based insurance are tethered to jobs for fear of losing their medical coverage while rural communities with high unemployment lose out on job-based insurance benefits.
Critics of Medicare for All oppose a government funded health care system, wanting to preserve a for-profit model to increase competition, and assert that hospitals, already financially vulnerable in rural America, would lose more money and risk bankruptcy because private insurance, on which they rely for financial stability, reimburses at higher rates than Medicare. Proponents argue, however, that proposed single-payer legislation in the House and Senate would boost hospital reimbursements far beyond current levels, while establishing annual global hospital funds that could be increased to cover unexpected costs and grant applications for capital improvements. Supporters of single-payer point to the closure of over 100 rural hospitals since 2010, with over 400 also at risk of closure, as evidence of the failure of a for-profit health insurance system unaffordable to many rural residents and unsustainable for hospitals that rely on reimbursements from private insurance.
Proponents of a national health insurance program to replace for-profit health insurance argue adoption of a federally funded single-payer system allowing patients to choose their own doctor would reduce "structural racism" in health care that results in non-white Americans suffering higher mortality rates in underserved communities. Backers of single-payer or Medicare for All note that minorities and the poor, as well as rural residents, in general, are less able to afford private health insurance, and that those who can must pay high deductibles and co-payments that threaten families with financial ruin. In addition, they argue that those with employment-based insurance are tethered to jobs for fear of losing their medical coverage while rural communities with high unemployment lose out on job-based insurance benefits.
Critics of Medicare for All oppose a government funded health care system, wanting to preserve a for-profit model to increase competition, and assert that hospitals, already financially vulnerable in rural America, would lose more money and risk bankruptcy because private insurance, on which they rely for financial stability, reimburses at higher rates than Medicare. Proponents argue, however, that proposed single-payer legislation in the House and Senate would boost hospital reimbursements far beyond current levels, while establishing annual global hospital funds that could be increased to cover unexpected costs and grant applications for capital improvements. Supporters of single-payer point to the closure of over 100 rural hospitals since 2010, with over 400 also at risk of closure, as evidence of the failure of a for-profit health insurance system unaffordable to many rural residents and unsustainable for hospitals that rely on reimbursements from private insurance.
Public option to the Affordable Care Act (ACA)
 Proponents of a public option support expanding the Affordable Care Act to give consumers a choice; private for-profit health insurance or Medicare. Backers of the public option say the ACA has not gone far enough, noting that despite the United States spending a greater percentage of its GDP on health care than any other nation, there are still over 28-million people without health insurance, resulting in Americans in underserved communities dying for lack of affordable care or declaring bankruptcy because of mounting medical bills.
While advocates of a public option agree with single-payer proponents that the United States should provide universal health care, they disagree on the solution, asserting that Americans are not interested in a government-run health care system and want to be able to keep their private health insurance. Critics who support single-payer instead charge that offering a public option to compete with private insurance would create a two-tiered system of concierge versus minimal medical services, as private for-profit insurance companies use political muscle to deny coverage to the oldest and sickest Americans, thus shunting the more expensive patients onto a financially vulnerable public option. Medicare for All proponents also say a hybrid system of private insurance coupled with a public option would result in added bureaucracy and paperwork, and therefore fail to lower health care costs.
Those favoring a strictly for-profit health care model claim a public option, with lower hospital reimbursements than private insurance, would bankrupt rural hospitals dependent on higher reimbursements from commercial insurance vendors.
Proponents of a public option support expanding the Affordable Care Act to give consumers a choice; private for-profit health insurance or Medicare. Backers of the public option say the ACA has not gone far enough, noting that despite the United States spending a greater percentage of its GDP on health care than any other nation, there are still over 28-million people without health insurance, resulting in Americans in underserved communities dying for lack of affordable care or declaring bankruptcy because of mounting medical bills.
While advocates of a public option agree with single-payer proponents that the United States should provide universal health care, they disagree on the solution, asserting that Americans are not interested in a government-run health care system and want to be able to keep their private health insurance. Critics who support single-payer instead charge that offering a public option to compete with private insurance would create a two-tiered system of concierge versus minimal medical services, as private for-profit insurance companies use political muscle to deny coverage to the oldest and sickest Americans, thus shunting the more expensive patients onto a financially vulnerable public option. Medicare for All proponents also say a hybrid system of private insurance coupled with a public option would result in added bureaucracy and paperwork, and therefore fail to lower health care costs.
Those favoring a strictly for-profit health care model claim a public option, with lower hospital reimbursements than private insurance, would bankrupt rural hospitals dependent on higher reimbursements from commercial insurance vendors.
Higher medical reimbursements and tax credits for rural hospitals
Seema Verma, Administrator of theCenters for Medicare & Medicaid Services
The Centers for Medicare & Medicaid Services (CMS), is a federal agency within the United States Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer M ...
(CMS), explains wage index disparities between urban and rural hospitals that led to underfunding rural hospitals will no longer strictly determine Medicare and Medicaid reimbursements. Under new policy rules, struggling rural hospitals may be eligible for higher Medicare reimbursements which, according to CMS, can be used to attract more highly skilled medical professionals. In addition, CMS will expand rural telehealth services under Medicare Advantage, a privatized insurance program, and relax supervision requirements for physician assistants and radiologist assistants.
On the state level, in 2016 Georgia established a $60 billion tax credit program to allow hospital donors to write off 100% of their donation to support a rural hospital. An investigation by the state's Department of Audits and Accounts found, however, the donations were not benefiting the rural hospitals that need the funds the most because too much money was deposited in the bank accounts of third party partners. Lawmakers have also complained that tax credits have benefited at least one rural hospital with a $60 million profit margin.
Free standing emergency centers (FECs)
In light of large numbers of hospital closures, particularly in rural America where the lack of emergency room services spawn health care deserts, proponents of 24-hour free standing emergency centers (FECs) advocate for more FECs that, unlike Urgent Care centers, would expand offerings beyond primary care to include: *Advanced laboratory equipment (x-rays; CT scans) *Emergency trained doctors and nurses *Pre-arranged transfer for patients requiring hospitalization *Prolonged 24-hour observation care FECs can function as outpatient departments for existing hospitals or as independently owned entities. One obstacle to the establishment of additional independently run FECs is the inability to receive Medicare and Medicaid reimbursements afforded only to licensed hospitals. Some FECs have overcome this barrier by establishing licensed micro-hospitals with eight to ten inpatient beds in underserved regions. Another obstacle to growth of FECs in underserved areas is the preference of for-profit health systems to place FECs in dense urban communities that will attract more patients and generate more money while replacing hospital-based emergency services and primary care. Advocates of the FEC model for hard-pressed communities argue the federal government should expand the recognition of independent FECs as Medicare and Medicaid participants in underserved areas.Telehealth
To address the rural health care crisis, advocates of telehealth promote the use of digital information and communication technology—cell phones and computers—that can be accessed from home or work without encumbering the patient with long travel times to hospitals at least 60 miles from their residence. Proponents say telehealth or remote medical attention can provide patients in health care deserts with greater access to specialists unavailable in rural communities while encouraging patients to assume a greater role in managing their own health care and improving communication between them and their team of doctors. For example, with telehealth a diabetic patient might: *Video conference with a doctor or other medical professional *Download an app to estimate, based on diet and activity, the amount of insulin needed. *Use a cell phone to upload food diaries and blood sugar levels for review by medical professionals *Watch a video on carbohydrate counting to better control glucose levels *Access an on-line patient portal to view test results, request pharmacy prescriptions, email a doctor or schedule an appointment *Receive email reminders to obtain a flu shot or other preventative careThe Heritage Foundation
The Heritage Foundation (abbreviated to Heritage) is an American conservative think tank based in Washington, D.C. that is primarily geared toward public policy. The foundation took a leading role in the conservative movement during the presiden ...
, a think tank advocating limited government, advocates for removal of federal obstacles in order to classify telehealth as preventative care under high deductible insurance plans, provide reimbursements for telehealth visits equal to in-person doctor visits and permit doctors licensed in one state to practice telemedicine across state lines.
Critics of telehealth argue on-line doctor visits are no substitute for in-person evaluations which can provide a more accurate diagnosis and that uninsured rural Americans still won't be able to afford quality medical care. In addition, they argue large swaths of rural America may not have access to broadband internet necessary for successful implementation of telehealth.
Incentives to recruit skilled medical professionals
The federalOffice of Rural Health Policy
The Office of Rural Health Policy (ORHP) is a part of the Health Resources and Services Administration (HRSA), of the United States Department of Health and Human Services (HHS).
Overview
HRSA is the lead federal agency responsible for monitori ...
oversees the non-profit National Rural Recruitment and Retention Network to connect medical professionals, hospitals and clinics in rural areas with recruitment and retention resources. The Network lists the following incentives rural legislative and medical entities could offer prospective doctors: health insurance, retirement packages, sabbaticals, sign-on bonuses, low-interest home loans. The Indian Health Service (IHS) offers prospective doctors up to $40,000 for repayment of student loans in exchange for a two-year commitment to serve American Indian and Alaska Native communities. Similarly, the National Health Service Corps (NHSC) offers up to $50,000 toward loan repayment if licensed health care providers agree to practice for two years in an underserved area. Under the federal NIMHD Loan Repayment Program (LRP) health professionals with doctoral degrees can receive up to $50,000 per year for two years to conduct research on health disparities.
See also
* Health in the United States *Healthcare in the United States
The United States far outspends any other nation on health care, measured both in ''per capita'' spending and as a percentage of GDP. Despite this, the country has significantly worse healthcare outcomes when compared to peer nations. The Uni ...
*Physician shortage in the United States
Concerns of a current and future shortage of medical doctors due to the supply and demand for physicians in the United States have come from multiple entities including professional bodies such as the American Medical Association (AMA), with the s ...
References
{{reflist Healthcare in the United States Social problems in medicine