intrauterine system on:
[Wikipedia]
[Google]
[Amazon]
A hormonal intrauterine device (IUD), also known as a intrauterine system (IUS) with progestogen and sold under the brand name Mirena among others, is an intrauterine device that releases a
 The hormonal IUD is a small 'T'-shaped piece of plastic, which contains
The hormonal IUD is a small 'T'-shaped piece of plastic, which contains

 The hormonal IUD is inserted in a similar procedure to the nonhormonal copper IUD, and can only be inserted by a qualified medical practitioner. Before insertion, a pelvic exam is performed to examine the shape and position of the uterus. A current STI at the time of insertion can increase the risk of pelvic infection. However, routine screening for gonorrhea and
The hormonal IUD is inserted in a similar procedure to the nonhormonal copper IUD, and can only be inserted by a qualified medical practitioner. Before insertion, a pelvic exam is performed to examine the shape and position of the uterus. A current STI at the time of insertion can increase the risk of pelvic infection. However, routine screening for gonorrhea and
Physician Fact Sheet (2008 U.S. version)
Physician Fact Sheet (2013 U.K. version)
Video showing the insertion procedure for a Mirena IUD
{{Portal bar, Medicine Hormonal contraception Bayer brands AbbVie brands World Health Organization essential medicines Wikipedia medicine articles ready to translate no:Hormonspiral
progestogen
Progestogens, also sometimes written progestagens or gestagens, are a class of natural or synthetic steroid hormones that bind to and activate the progesterone receptors (PR). Progesterone is the major and most important progestogen in the body ...
ic hormonal agent
A hormone (from the Greek participle , "setting in motion") is a class of signaling molecules in multicellular organisms that are sent to distant organs by complex biological processes to regulate physiology and behavior. Hormones are required fo ...
such as levonorgestrel
Levonorgestrel is a hormonal medication which is used in a number of birth control methods. It is combined with an estrogen to make combination birth control pills. As an emergency birth control, sold under the brand name Plan B One-Step among ...
into the uterus. It is used for birth control
Birth control, also known as contraception, anticonception, and fertility control, is the use of methods or devices to prevent unwanted pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth contr ...
, heavy menstrual periods, and to prevent excessive build of the lining of the uterus in those on estrogen replacement therapy
Hormone replacement therapy (HRT), also known as menopausal hormone therapy or postmenopausal hormone therapy, is a form of hormone therapy used to treat symptoms associated with female menopause. These symptoms can include hot flashes, vaginal ...
. It is one of the most effective forms of birth control with a one-year failure rate around 0.2%. The device is placed in the uterus and lasts three to eight years. Fertility often returns quickly following removal.
Side effects include irregular periods, benign ovarian cysts
An ovarian cyst is a fluid-filled sac within the ovary. Often they cause no symptoms. Occasionally they may produce bloating, lower abdominal pain, or lower back pain. The majority of cysts are harmless. If the cyst either breaks open or causes ...
, pelvic pain, and depression. Rarely uterine perforation
Uterine perforation is a potential complication of any intrauterine procedure. It may be associated with injury to surrounding blood vessels or viscera such as the bladder or intestine. If not diagnosed at the time of the procedure it can occasion ...
may occur. Use is not recommended during pregnancy but is safe with breastfeeding
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant. The World Health Organization (WHO) recommends that brea ...
. The IUD with progestogen is a type of long-acting reversible birth control. It works by thickening the mucus at the opening of the cervix
The cervix or cervix uteri (Latin, 'neck of the uterus') is the lower part of the uterus (womb) in the human female reproductive system. The cervix is usually 2 to 3 cm long (~1 inch) and roughly cylindrical in shape, which changes during ...
, stopping the buildup of the lining of the uterus, and occasionally preventing ovulation
Ovulation is the release of eggs from the ovaries. In women, this event occurs when the ovarian follicles rupture and release the secondary oocyte ovarian cells. After ovulation, during the luteal phase, the egg will be available to be fertilize ...
.
The IUD with levonorgestrel was first approved for medical use in 1990 in Finland and in the United States in 2000. It is on the World Health Organization's List of Essential Medicines.
Medical uses
The hormonal IUD is an extremely effective method ofbirth control
Birth control, also known as contraception, anticonception, and fertility control, is the use of methods or devices to prevent unwanted pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth contr ...
, and a 2021 study demonstrated that it may be used for emergency contraception
Emergency contraception (EC) is a birth control measure, used after sexual intercourse to prevent pregnancy.
There are different forms of EC. Emergency contraceptive pills (ECPs), sometimes simply referred to as emergency contraceptives (ECs), ...
. In addition to birth control, the hormonal IUD is used for prevention and treatment of:
* Heavy menstrual periods
* Endometriosis
Endometriosis is a disease of the female reproductive system in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus. Most often this is on the ovaries, fall ...
and chronic pelvic pain
Pelvic pain is pain in the area of the pelvis. Acute pain is more common than chronic pain. If the pain lasts for more than six months, it is deemed to be chronic pelvic pain. It can affect both the male and female pelvis.
Common causes in include ...
* Adenomyosis
Adenomyosis is a medical condition characterized by the growth of cells that proliferate on the inside of the uterus (endometrium) atypically located among the cells of the uterine wall (myometrium), as a result, thickening of the uterus occurs. A ...
and dysmenorrhea
Dysmenorrhea, also known as period pain, painful periods or menstrual cramps, is pain during menstruation. Its usual onset occurs around the time that menstruation begins. Symptoms typically last less than three days. The pain is usually in the ...
* Anemia
Anemia or anaemia (British English) is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, t ...
* Endometrial hyperplasia
Endometrial hyperplasia is a condition of excessive proliferation of the cells of the endometrium, or inner lining of the uterus.
Most cases of endometrial hyperplasia result from high levels of estrogens, combined with insufficient levels of th ...
(especially in pre-menopausal women who wish to maintain fertility in the treatment of endometrial hyperplasia)
* In some cases, use of a hormonal IUD may prevent a need for a hysterectomy.
Advantages:
* Considered one of the most effective forms of reversible birth control
* Can be used while breastfeeding (see also nursing mothers)
* No preparations needed before sex, though routine checking of the device strings by patient and physician is advised to ensure proper placement remains intact
* 90% of users who wish to become pregnant do so within 24 months of removal.
* May experience lighter periods (some women stop having periods completely, see also amenorrhea
Amenorrhea is the absence of a menstrual period in a woman of reproductive age. Physiological states of amenorrhoea are seen, most commonly, during pregnancy and lactation (breastfeeding). Outside the reproductive years, there is absence of menses ...
)
* Effective for up to three to eight years (depending on the IUD)
Disadvantages:
* Irregular periods and spotting between periods often occurs after insertion This usually improves after three to six months.
* Moderate to severe discomfort may be experienced during insertion procedure, including uterine cramping and back pain.
* Other potential adverse effects
An adverse effect is an undesired harmful effect resulting from a medication or other intervention, such as surgery. An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. The term complica ...
and risks
Effectiveness
After insertion, Mirena is effective at preventing pregnancy for up to seven years. Kyleena is approved for five years and Skyla is approved for three years. The hormonal IUD is a long-acting reversible contraceptive, and is considered one of the most effective forms of birth control. The first year failure rate for the hormonal IUD is 0.1-0.2% and the five-year failure rate is 0.7-0.9%. These rates are comparable to tubal sterilization, but unlike sterilization the effects of the hormonal IUD are reversible. The hormonal IUD is considered to be more effective than other common forms of reversible contraception, such as thebirth control pill
The combined oral contraceptive pill (COCP), often referred to as the birth control pill or colloquially as "the pill", is a type of birth control that is designed to be taken orally by women. The pill contains two important hormones: progesti ...
, because it requires little action by the user after insertion. The effectiveness of other forms of birth control is mitigated (decreased) by the users themselves. If medication regimens for contraception are not followed precisely, the method becomes less effective. IUDs require no daily, weekly, or monthly regimen, so their typical use failure rate is therefore the same as their perfect use failure rate.
In women with bicornuate uterus
A bicornuate uterus or bicornate uterus (from the Latin ''cornū'', meaning "horn"), is a type of mullerian anomaly in the human uterus, where there is a deep indentation at the fundus (top) of the uterus.
Pathophysiology
A bicornuate uterus ...
and in need of contraception, two IUDs are generally applied (one in each horn) due to lack of evidence of efficacy with only one IUD. Evidence is lacking regarding progestogen IUD usage for menorrhagia
Heavy menstrual bleeding (HMB), previously known as menorrhagia or hypermenorrhea, is a menstrual period with excessively heavy flow. It is a type of abnormal uterine bleeding (AUB).
Abnormal uterine bleeding can be caused by structural abnorma ...
in bicornuate uterus, but a case report showed good effect with a single IUD for this purpose.
Breastfeeding
Progestogen-only contraceptives such as an IUD are not believed to affect milk supply or infant growth. However, a study in the Mirena application for FDA approval found a lower continuation of breastfeeding at 75 days in hormonal IUD users (44%) versus copper IUD users (79%).FDA Medical Review p. 37. When using Mirena, about 0.1% of the maternal dose of levonorgestrel can be transferred via milk to the nursed infant. A six-year study of breastfed infants whose mothers used a levonorgestrel-only method of birth control found the infants had increased risk of respiratory infections and eye infections, though a lower risk of neurological conditions, compared to infants whose mothers used a copper IUD. No longer-term studies have been performed to assess the long-term effects on infants of levonorgestrel in breast milk. There are conflicting recommendations about use of Mirena while breastfeeding. The U.S. CDC does not recommend any hormonal method as a first choice of contraceptive for nursing mothers, although progestin-only methods, such as Mirena, may be used with close follow-up or when the benefits outweigh the risks. The World Health Organization recommends against immediate postpartum insertion, citing increased expulsion rates. It also reports concerns about potential effects on the infant's liver and brain development in the first six weeks postpartum. However, it recommends offering Mirena as a contraceptive option beginning at six weeks postpartum even to nursing women. Planned Parenthood offers Mirena as a contraceptive option for breastfeeding women beginning at four weeks postpartum.Contraindications
A hormonal IUD should not be used by women who: * Are, or think they may be, pregnant * Have abnormal vaginal bleeding that has not been explained (controversial) * Have untreated cervical or uterine cancer * Have, or may have,breast cancer
Breast cancer is cancer that develops from breast tissue. Signs of breast cancer may include a lump in the breast, a change in breast shape, dimpling of the skin, milk rejection, fluid coming from the nipple, a newly inverted nipple, or a r ...
* Have abnormalities of the cervix
The cervix or cervix uteri (Latin, 'neck of the uterus') is the lower part of the uterus (womb) in the human female reproductive system. The cervix is usually 2 to 3 cm long (~1 inch) and roughly cylindrical in shape, which changes during ...
or uterus (controversial)
* Have had pelvic inflammatory disease
Pelvic inflammatory disease, also known as pelvic inflammatory disorder (PID), is an infection of the upper part of the female reproductive system, namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis. Often, there may be n ...
within the past three months
* Have had an STI such as chlamydia
Chlamydia, or more specifically a chlamydia infection, is a sexually transmitted infection caused by the bacterium ''Chlamydia trachomatis''. Most people who are infected have no symptoms. When symptoms do appear they may occur only several wee ...
or gonorrhea within the past three months
* Have liver disease or tumor
* Have an allergy to levonorgestrel
Levonorgestrel is a hormonal medication which is used in a number of birth control methods. It is combined with an estrogen to make combination birth control pills. As an emergency birth control, sold under the brand name Plan B One-Step among ...
or any of the inactive ingredients included in the device
Insertion of an IUD is acceptable after a dilation and evacuation
Dilation and evacuation (D&E) is the dilation of the cervix and surgical evacuation of the uterus (potentially including the fetus, placenta and other tissue) after the first trimester of pregnancy. It is a method of abortion as well as a common ...
(D&E) abortion (second-trimester abortion), but may be associated with a higher expulsion rate. To reduce the risk of infection, insertion of an IUD is not recommended for women that have had a medical abortion
A medical abortion, also known as medication abortion, occurs when drugs (medication) are used to bring about an abortion. Medical abortions are an alternative to surgical abortions such as vacuum aspiration or dilation and curettage. Medical ...
but have not yet had an ultrasound to confirm that the abortion was complete, or that have not yet had their first menstruation following the medical abortion.
A full list of contraindications can be found in the WHO ''Medical Eligibility Criteria for Contraceptive Use'' and the CDC
The Centers for Disease Control and Prevention (CDC) is the national public health agency of the United States. It is a United States federal agency, under the Department of Health and Human Services, and is headquartered in Atlanta, Georg ...
''United States Medical Eligibility Criteria for Contraceptive Use''.
Side effects
* Irregular menstrual pattern: irregular bleeding and spotting is common in the first three to six months of use. After that time periods become shorter and lighter, and 20% of women stop having periods after one year of use. The average user reports 16 days of bleeding or spotting in the first month of use, but this diminishes to about four days at 12 months. * Cramping and pain: many women feel discomfort or pain during and immediately after insertion. Some women may have cramping for the first 1–2 weeks after insertion. * Expulsion: Sometimes the IUD can slip out of the uterus. This is termed expulsion. Around 5% of IUD users experience expulsion. If this happens a woman is not protected from pregnancy. Expulsion is more common in younger women, women who have not had children, and when an IUD is inserted immediately after childbirth or abortion. * Perforation: Very rarely, the IUD can be pushed through the wall of the uterus during insertion. Risk of perforation is mostly determined by the skill of the practitioner performing the insertion. For experienced medical practitioners, the risk of perforation is one per 1,000 insertions or less. With postpartum insertions, perforation of the uterus is more likely to occur when uterine involution is incomplete; involution usually completes by 4–6 weeks postpartum. Special considerations apply to women who plan tobreastfeed
Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant. The World Health Organization (WHO) recommends that brea ...
. If perforation does occur it can damage the internal organs, and in some cases surgery is needed to remove the IUD.
* Pregnancy complications: Although the risk of pregnancy with an IUD is very small, if one does occur there is an increased risk of serious problems. These include ectopic pregnancy
Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus. Signs and symptoms classically include abdominal pain and vaginal bleeding, but fewer than 50 percent of affected women have both of these symptoms. ...
, infection, miscarriage, and early labor and delivery. As many as half the pregnancies that occur in Mirena users may be ectopic. The incidence rate of ectopic pregnancies is approximately one per 1000 users per year. Immediate removal of the IUD is recommended in the case of pregnancy. No pattern of birth defects was found in the 35 babies for whom birth outcomes were available at the time of FDA approval.
* Infection: The insertion of the IUD does have a small risk of pelvic inflammatory disease
Pelvic inflammatory disease, also known as pelvic inflammatory disorder (PID), is an infection of the upper part of the female reproductive system, namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis. Often, there may be n ...
(PID). Concurrent infection with gonorrhea or chlamydia
Chlamydia, or more specifically a chlamydia infection, is a sexually transmitted infection caused by the bacterium ''Chlamydia trachomatis''. Most people who are infected have no symptoms. When symptoms do appear they may occur only several wee ...
at the time of insertion increases the risk of pelvic inflammatory disease. If PID does occur, it will most likely happen within 21 days of insertion. The device itself does not increase the risk of infection.
* Ovarian cyst
An ovarian cyst is a fluid-filled sac within the ovary. Often they cause no symptoms. Occasionally they may produce bloating, lower abdominal pain, or lower back pain. The majority of cysts are harmless. If the cyst either breaks open or causes ...
s: Enlarged follicles (ovarian cysts) have been diagnosed in about 12% of the subjects using a hormonal IUD in studies that use ultrasound to look for cysts, even if asymptomatic. In studies that only evaluate symptomatic cysts, only 4.5% of women complain of any ovarian cysts over 5 or more years of use, and only 0.3% require IUD removal for ovarian cysts. Thus, any issues with ovarian cysts are not of a clinically relevant nature. Most of these follicles are asymptomatic, although some may be accompanied by pelvic pain or dyspareunia. In most cases the enlarged follicles disappear spontaneously after two to three months. Surgical intervention is not usually required.
* Mental health changes including: nervousness, depressed mood, mood swings
* Weight gain
* Headache, migraine
* Nausea
* Acne
* Excessive hairiness
* Lower abdominal or back pain
* Decreased libido
* Itching, redness or swelling of the vagina
* Vaginal discharge
* Breast pain, tenderness
* Edema
* Abdominal distension
* Cervicitis
Cervicitis is inflammation of the uterine cervix. Cervicitis in women has many features in common with urethritis in men and many cases are caused by sexually transmitted infections. Non-infectious causes of cervicitis can include intrauterine d ...
* Bacterial vaginosis
Bacterial vaginosis (BV) is a disease of the vagina caused by excessive growth of bacteria. Common symptoms include increased vaginal discharge that often smells like fish. The discharge is usually white or gray in color. Burning with urinati ...
* May affect glucose tolerance
* May experience a change in vision or contact lens tolerance
* May deplete vitamin B1 which can affect energy, mood, and nervous system functioning
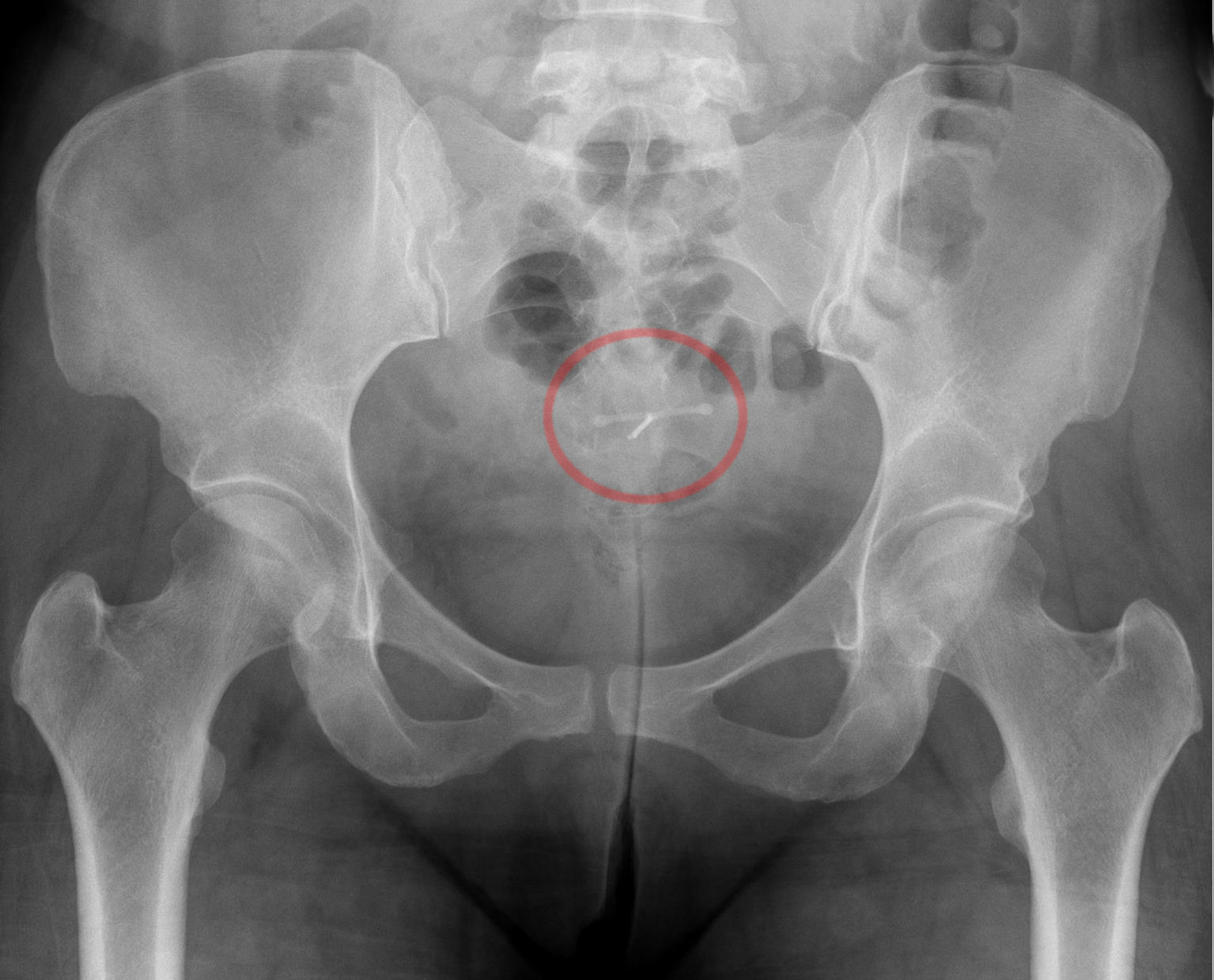
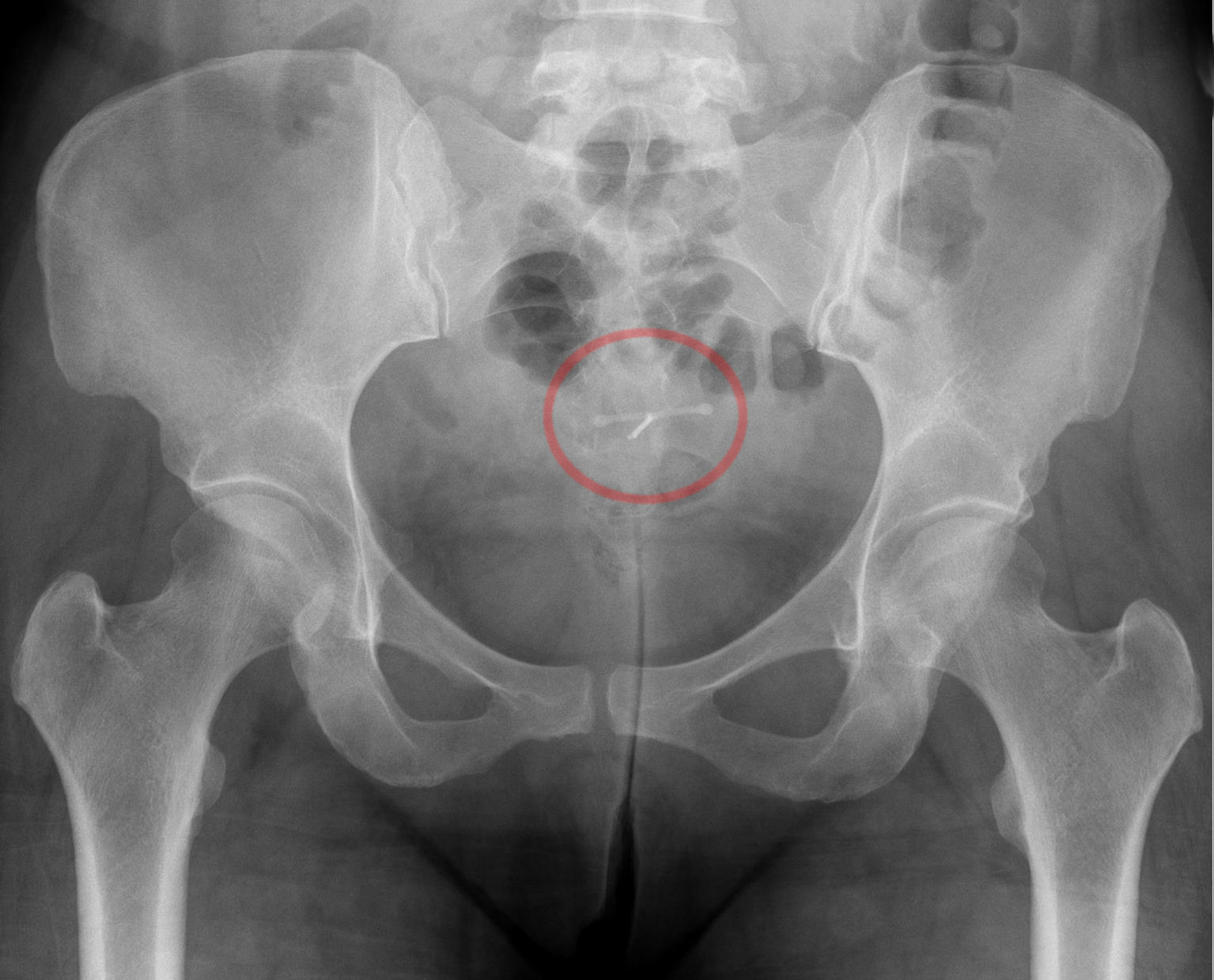
* A "lost coil" occurs when the thread cannot be felt by a woman on routine checking and is not seen on speculum examination. Various thread collector devices or simple forceps may then be used to try to grasp the device through the cervix. In the rare cases when this is unsuccessful, an ultrasound scan may be arranged to check the position of the coil and exclude its perforation through into the abdominal cavity or its unrecognised previous expulsion.
Cancer
According to a 1999 evaluation of the studies performed on progestin-only birth control by the International Agency for Research on Cancer, there is some evidence that progestin-only birth control reduces the risk of endometrial cancer. The IARC in 1999 concluded that there is no evidence progestin-only birth control increases the risk of any cancer, though the available studies were too small to be definitively conclusive. Progesterone is a hormone in the endometrium that counteracts estrogen driven growth. Very low levels of progesterone will cause estrogen to act more, leading to endometrial hyperplasia and adenocarcinoma. These effects can be minimized if treated with progestin, but not in very many cases. Estrogen and progesterone have an antagonistic relationship. Estrogen promotes the growing of endometrial lining, while progesterone limits it. In the case of endometrial cancer, progesterone can negatively regulate estrogen driven growth. Tumors formed are correlated with insufficient progesterone and excess estrogen. In patients with endometrial cancer who use progestin releasing IUDs concluded mixed results. A 2020 meta-analysis by Livia Conz et al. estimated that users of levonorgestrel-releasing systems had an increased breast cancer risk in general (with anodds ratio
An odds ratio (OR) is a statistic that quantifies the strength of the association between two events, A and B. The odds ratio is defined as the ratio of the odds of A in the presence of B and the odds of A in the absence of B, or equivalently (due ...
of 1.16) and higher risk for those over age 50 (odds ratio 1.52), and suggested balancing this risk against the known benefits of long-term use. Researchers cautioned against causal interpretation from this study, citing confounding
In statistics, a confounder (also confounding variable, confounding factor, extraneous determinant or lurking variable) is a variable that influences both the dependent variable and independent variable, causing a spurious association. Con ...
effects, methodological concerns and a 2020 meta-analysis of randomized controlled trials which showed no increased risk.
Bone density
No evidence has been identified to suggest Mirena affects bone mineral density (BMD). Two small studies, limited to studying BMD in the forearm, show no decrease in BMD. One of the studies showed at seven years of use, similar BMD at the midshaft of theulna
The ulna (''pl''. ulnae or ulnas) is a long bone found in the forearm that stretches from the elbow to the smallest finger, and when in anatomical position, is found on the medial side of the forearm. That is, the ulna is on the same side of t ...
and at the distal radius as nonusers matched by age and BMI. In addition, BMD measurements were similar to the expected values for women in the same age group as the participants. The authors of the study said their results were predictable, since it is well established that the main factor responsible for bone loss in women is hypoestrogenism
Hypoestrogenism, or estrogen deficiency, refers to a lower than normal level of estrogen. It is an umbrella term used to describe estrogen deficiency in various conditions. Estrogen deficiency is also associated with an increased risk of cardiova ...
, and, in agreement with previous reports, they found estradiol
Estradiol (E2), also spelled oestradiol, is an estrogen steroid hormone and the major female sex hormone. It is involved in the regulation of the estrous and menstrual female reproductive cycles. Estradiol is responsible for the development of ...
levels in Mirena users to be normal.
Composition and hormonal release
 The hormonal IUD is a small 'T'-shaped piece of plastic, which contains
The hormonal IUD is a small 'T'-shaped piece of plastic, which contains levonorgestrel
Levonorgestrel is a hormonal medication which is used in a number of birth control methods. It is combined with an estrogen to make combination birth control pills. As an emergency birth control, sold under the brand name Plan B One-Step among ...
, a type of progestin., Bayer Pharmaceuticals. The cylinder of the device is coated with a membrane that regulates the release of the drug. Bayer markets Skyla as Jaydess in the United Kingdom. Jaydess releases six micrograms per day and lasts for three years. In comparison, oral contraceptives can contain 150 micrograms of levonorgestrel. p.150: The hormonal IUD releases the levonorgestrel directly into the uterus, as such its effects are mostly paracrine Paracrine signaling is a form of cell signaling, a type of cellular communication in which a cell produces a signal to induce changes in nearby cells, altering the behaviour of those cells. Signaling molecules known as paracrine factors diffuse ove ...
rather than systemic. Most of the drug stays inside the uterus, and only a small amount is absorbed into the rest of the body.
Insertion and removal

 The hormonal IUD is inserted in a similar procedure to the nonhormonal copper IUD, and can only be inserted by a qualified medical practitioner. Before insertion, a pelvic exam is performed to examine the shape and position of the uterus. A current STI at the time of insertion can increase the risk of pelvic infection. However, routine screening for gonorrhea and
The hormonal IUD is inserted in a similar procedure to the nonhormonal copper IUD, and can only be inserted by a qualified medical practitioner. Before insertion, a pelvic exam is performed to examine the shape and position of the uterus. A current STI at the time of insertion can increase the risk of pelvic infection. However, routine screening for gonorrhea and chlamydia
Chlamydia, or more specifically a chlamydia infection, is a sexually transmitted infection caused by the bacterium ''Chlamydia trachomatis''. Most people who are infected have no symptoms. When symptoms do appear they may occur only several wee ...
prior to insertion is not recommended. If a person needs screening and there is no evidence of infection on examination or has been previously screened, insertion of the IUD does not need to be delayed.
Insertion
During the insertion, the vagina is held open with a speculum, the same device used during a pap smear. A grasping instrument is used to steady the cervix, the length of the uterus is measured for proper insertion with a uterine sound for decreasing chance of uterine perforation with the IUD, and the IUD is placed using a narrow tube through the opening of the cervix into the uterus. A short length of monofilament plastic/nylon string hangs down from the cervix into the vagina. The string allows physicians and patients to check to ensure the IUD is still in place and enables easy removal of the device. Mild to moderate cramping can occur during the procedure, which generally takes five minutes or less. Insertion can be performed immediately postpartum and post-abortion if no infection has occurred. Misoprostol is not effective in reducing pain in IUD insertion.Removal
Removal of the device should also be performed by a qualified medical practitioner. After removal, fertility will return to previous levels relatively quickly. One study found that the majority of participants returned to fertility within three months.Mechanisms of action
Levonorgestrel is aprogestogen
Progestogens, also sometimes written progestagens or gestagens, are a class of natural or synthetic steroid hormones that bind to and activate the progesterone receptors (PR). Progesterone is the major and most important progestogen in the body ...
, i.e. a progesterone receptor agonist
An agonist is a chemical that activates a receptor to produce a biological response. Receptors are cellular proteins whose activation causes the cell to modify what it is currently doing. In contrast, an antagonist blocks the action of the ago ...
. The hormonal IUD's primary mechanism of action
In pharmacology, the term mechanism of action (MOA) refers to the specific biochemical interaction through which a drug substance produces its pharmacological effect. A mechanism of action usually includes mention of the specific molecular targ ...
is to prevent fertilization
Fertilisation or fertilization (see spelling differences), also known as generative fertilisation, syngamy and impregnation, is the fusion of gametes to give rise to a new individual organism or offspring and initiate its development. Proce ...
. p. S28: p. 199: pp. 246–247: p. 259: The levonorgestrel intrauterine system has several contraceptive effects, although thickening of the cervical mucus appears to be the primary effect. Other effects include making the inside of the uterus become fatal to sperm and thinning of the endometrial lining, but this is not the usual function.
Ovulation is not inhibited in all cases.
Numerous studies have demonstrated that IUDs primarily prevent fertilization, not implantation. In one experiment involving tubal flushing, fertilized eggs were found in half of women not using contraception, but no fertilized eggs were found in women using IUDs. IUDs also decrease the risk of ectopic pregnancy, which further implies that IUDs prevent fertilization.
History
Hormonal IUDs were developed in the 1970s following the development of the copper IUD in the 1960s and 1970s. Dr. Antonio Scommenga, working at the Michael Reese Hospital in Chicago, discovered that administering progesterone inside the uterus could have contraceptive benefits. With knowledge of Scommegna's work, a Finnish doctor, Jouni Valter Tapani Luukkainen, created the 'T'-shaped IUD that released progesterone, marketed as the Progestasert System in 1976. This IUD had a short, 1-year lifespan and never achieved widespread popularity. Following this relative lack of success, Dr. Luukkainen replaced the progesterone with the hormone levonorgestrel to be released over a five-year period, creating what is now Mirena. The Mirena IUD was studied for safety and efficacy in two clinical trials in Finland and Sweden involving 1,169 women who were all between 18 and 35 years of age at the beginning of the trials. The trials included predominantly Caucasian women who had been previously pregnant with no history of ectopic pregnancy or pelvic inflammatory disease within the previous year. Over 70% of the participants had previously used IUDs. In 2013 Skyla, a lower dose levonorgestrel IUD effective for up to three years, was approved by the FDA. Skyla has a different bleeding pattern than Mirena, with only 6% of women in clinical trials becoming amenorrheic (compared to approximately 20% with Mirena). The city of Finland, Turku, is currently the only production site for the Mirena contraceptive family.Controversies
In 2009,Bayer
Bayer AG (, commonly pronounced ; ) is a German multinational pharmaceutical and biotechnology company and one of the largest pharmaceutical companies in the world. Headquartered in Leverkusen, Bayer's areas of business include pharmaceutica ...
, the maker of Mirena, was issued an FDA Warning Letter An FDA warning letter is an official message from the United States Food and Drug Administration (FDA) to a manufacturer or other organization that has violated some rule in a federally regulated activity.
The FDA defines an FDA warning letter as ...
by the United States Food and Drug Administration for overstating the efficacy, minimizing the risks of use, and making "false or misleading presentations" about the device. From 2000 to 2013, the federal agency received over 70,072 complaints about the device and related adverse effects. As of April 2014, over 1,200 lawsuits have been filed in the United States.
References
External links
* - on Berlex Laboratories' Mirena applicationPhysician Fact Sheet (2008 U.S. version)
Physician Fact Sheet (2013 U.K. version)
Video showing the insertion procedure for a Mirena IUD
{{Portal bar, Medicine Hormonal contraception Bayer brands AbbVie brands World Health Organization essential medicines Wikipedia medicine articles ready to translate no:Hormonspiral