emergency departments on:
[Wikipedia]
[Google]
[Amazon]
 An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in
An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in
File:Emergency room sign.jpg,


 All accident and emergency (A&E) departments throughout the United Kingdom are financed and managed publicly by the National Health Service (NHS of each constituent country ( England, Scotland, Wales and Northern Ireland). The term "A&E" is widely recognised and used rather than the full name; it is used on road signs, official documentation, etc.
A&E services are provided to all, without charge. Other NHS medical care, including hospital treatment following an emergency, is free of charge only to all who are "ordinarily resident" in Britain; residency rather than citizenship is the criterion (details on charges vary from country to country).
In England departments are divided into three categories:
* Type 1 department – major A&E, providing a consultant-led 24 hour service with full resuscitation facilities
* Type 2 department – single specialty A&E service (e.g. ophthalmology, dentistry)
* Type 3 department – other A&E/minor injury unit/walk-in centre, treating minor injuries and illnesses
Historically, waits for assessment in A&E were very long in some areas of the UK. In October 2002, the Department of Health introduced a four-hour target in emergency departments that required departments in England to assess and treat patients within four hours of arrival, with referral and assessment by other departments if deemed necessary. It was expected that the patients would have physically left the department within the four hours. Present policy is that 95% of all patient cases do not "breach" this four-hour wait. The busiest departments in the UK outside London include University Hospital of Wales in Cardiff, The North Wales Regional Hospital in Wrexham, the Royal Infirmary of Edinburgh and Queen Alexandra Hospital in Portsmouth.
In July 2014, the QualityWatch research programme published in-depth analysis which tracked 41 million A&E attendances from 2010 to 2013. This showed that the number of patients in a department at any one time was closely linked to waiting times, and that crowding in A&E had increased as a result of a growing and ageing population, compounded by the freezing or reduction of A&E capacity. Between 2010/11 and 2012/13 crowding increased by 8%, despite a rise of just 3% in A&E visits, and this trend looks set to continue. Other influential factors identified by the report included temperature (with both hotter and colder weather pushing up A&E visits), staffing and inpatient bed numbers.
A&E services in the UK are often the focus of a great deal of media and political interest, and data on A&E performance is published weekly. However, this is only one part of a complex urgent and emergency care system. Reducing A&E waiting times therefore requires a comprehensive, coordinated strategy across a range of related services.
Many A&E departments are crowded and confusing. Many of those attending are understandably anxious, and some are mentally ill, and especially at night are under the influence of alcohol or other substances. Pearson Lloyd's redesign – 'A Better A&E' – is claimed to have reduced aggression against hospital staff in the departments by 50 per cent. A system of environmental signage provides location-specific information for patients. Screens provide live information about how many cases are being handled and the current status of the A&E department. Waiting times for patients to be seen at A&E were rising in the years leading up to 2020, and were hugely worsened during the covid-19 pandemic that started in 2020.
In response to the year-on-year increasing pressure on A&E units, followed by the unprecedented effects of the covid-19 pandemic, the NHS in late 2020 proposed a radical change to handling of urgent and emergency care,
separating "emergency" and "urgent". Emergencies are . Urgent requirements are for . As part of the response, walk-in Urgent Treatment Centres (UTC) were created. People potentially needing A&E treatment are recommended to phone the NHS111 line, which will either book an arrival time for A&E, or recommend a more appropriate procedure. (Information is for England; details may vary in different countries.)
All accident and emergency (A&E) departments throughout the United Kingdom are financed and managed publicly by the National Health Service (NHS of each constituent country ( England, Scotland, Wales and Northern Ireland). The term "A&E" is widely recognised and used rather than the full name; it is used on road signs, official documentation, etc.
A&E services are provided to all, without charge. Other NHS medical care, including hospital treatment following an emergency, is free of charge only to all who are "ordinarily resident" in Britain; residency rather than citizenship is the criterion (details on charges vary from country to country).
In England departments are divided into three categories:
* Type 1 department – major A&E, providing a consultant-led 24 hour service with full resuscitation facilities
* Type 2 department – single specialty A&E service (e.g. ophthalmology, dentistry)
* Type 3 department – other A&E/minor injury unit/walk-in centre, treating minor injuries and illnesses
Historically, waits for assessment in A&E were very long in some areas of the UK. In October 2002, the Department of Health introduced a four-hour target in emergency departments that required departments in England to assess and treat patients within four hours of arrival, with referral and assessment by other departments if deemed necessary. It was expected that the patients would have physically left the department within the four hours. Present policy is that 95% of all patient cases do not "breach" this four-hour wait. The busiest departments in the UK outside London include University Hospital of Wales in Cardiff, The North Wales Regional Hospital in Wrexham, the Royal Infirmary of Edinburgh and Queen Alexandra Hospital in Portsmouth.
In July 2014, the QualityWatch research programme published in-depth analysis which tracked 41 million A&E attendances from 2010 to 2013. This showed that the number of patients in a department at any one time was closely linked to waiting times, and that crowding in A&E had increased as a result of a growing and ageing population, compounded by the freezing or reduction of A&E capacity. Between 2010/11 and 2012/13 crowding increased by 8%, despite a rise of just 3% in A&E visits, and this trend looks set to continue. Other influential factors identified by the report included temperature (with both hotter and colder weather pushing up A&E visits), staffing and inpatient bed numbers.
A&E services in the UK are often the focus of a great deal of media and political interest, and data on A&E performance is published weekly. However, this is only one part of a complex urgent and emergency care system. Reducing A&E waiting times therefore requires a comprehensive, coordinated strategy across a range of related services.
Many A&E departments are crowded and confusing. Many of those attending are understandably anxious, and some are mentally ill, and especially at night are under the influence of alcohol or other substances. Pearson Lloyd's redesign – 'A Better A&E' – is claimed to have reduced aggression against hospital staff in the departments by 50 per cent. A system of environmental signage provides location-specific information for patients. Screens provide live information about how many cases are being handled and the current status of the A&E department. Waiting times for patients to be seen at A&E were rising in the years leading up to 2020, and were hugely worsened during the covid-19 pandemic that started in 2020.
In response to the year-on-year increasing pressure on A&E units, followed by the unprecedented effects of the covid-19 pandemic, the NHS in late 2020 proposed a radical change to handling of urgent and emergency care,
separating "emergency" and "urgent". Emergencies are . Urgent requirements are for . As part of the response, walk-in Urgent Treatment Centres (UTC) were created. People potentially needing A&E treatment are recommended to phone the NHS111 line, which will either book an arrival time for A&E, or recommend a more appropriate procedure. (Information is for England; details may vary in different countries.)
 Medication errors are issues that lead to incorrect medication distribution or potential for patient harm. As of 2014, around 3% of all hospital-related adverse effects were due to medication errors in the emergency department (ED); between 4% and 14% of medications given to patients in the ED were incorrect and children were particularly at risk.
Errors can arise if the doctor prescribes the wrong medication, if the prescription intended by the doctor is not the one actually communicated to the
Medication errors are issues that lead to incorrect medication distribution or potential for patient harm. As of 2014, around 3% of all hospital-related adverse effects were due to medication errors in the emergency department (ED); between 4% and 14% of medications given to patients in the ED were incorrect and children were particularly at risk.
Errors can arise if the doctor prescribes the wrong medication, if the prescription intended by the doctor is not the one actually communicated to the
ED visits
(US) (National Center for Health Statistics)
Academic Emergency Medicine
, , Elsvier
Physicians on Call: California's Patchwork Approach to Emergency Department Coverage
Wait Time for Treatment in Hospital Emergency Departments, 2009.
Hyattsville, Md.:
 An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in
An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine
Emergency medicine is the medical speciality concerned with the care of illnesses or injuries requiring immediate medical attention. Emergency physicians (often called “ER doctors” in the United States) continuously learn to care for unsche ...
, the acute care of patients who present without prior appointment; either by their own means or by that of an ambulance. The emergency department is usually found in a hospital
A hospital is a health care institution providing patient treatment with specialized health science and auxiliary healthcare staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emerge ...
or other primary care center.
Due to the unplanned nature of patient attendance, the department must provide initial treatment for a broad spectrum of illnesses and injuries, some of which may be life-threatening and require immediate attention. In some countries, emergency departments have become important entry points for those without other means of access to medical care.
The emergency departments of most hospitals operate 24 hours a day, although staffing levels may be varied in an attempt to reflect patient volume.
History
Accident services were provided by workmen's compensation plans, railway companies, and municipalities in Europe and the United States by the late mid-nineteenth century, but the world's first specialized trauma care center was opened in 1911 in the United States at the University of Louisville Hospital in Louisville, Kentucky. It was further developed in the 1930s by surgeon Arnold Griswold, who also equipped police and fire vehicles with medical supplies and trained officers to give emergency care while en route to the hospital. Today, a typical hospital has its emergency department in its own section of the ground floor of the grounds, with its own dedicated entrance. As patients can arrive at any time and with any complaint, a key part of the operation of an emergency department is the prioritization of cases based on clinical need. This process is called triage. Triage is normally the first stage the patient passes through, and consists of a brief assessment, including a set of vital signs, and the assignment of a "chief complaint" (e.g. chest pain, abdominal pain, difficulty breathing, etc.). Most emergency departments have a dedicated area for this process to take place and may have staff dedicated to performing nothing but a triage role. In most departments, this role is fulfilled by a triage nurse, although dependent on training levels in the country and area, other health care professionals may perform the triage sorting, including paramedics and physicians. Triage is typically conducted face-to-face when the patient presents, or a form of triage may be conducted via radio with an ambulance crew; in this method, the paramedics will call the hospital's triage center with a short update about an incoming patient, who will then be triaged to the appropriate level of care. Most patients will be initially assessed at triage and then passed to another area of the department, or another area of the hospital, with their waiting time determined by their clinical need. However, some patients may complete their treatment at the triage stage, for instance, if the condition is very minor and can be treated quickly, if only advice is required, or if the emergency department is not a suitable point of care for the patient. Conversely, patients with evidently serious conditions, such as cardiac arrest, will bypass triage altogether and move straight to the appropriate part of the department. Theresuscitation
Resuscitation is the process of correcting physiological disorders (such as lack of breathing or heartbeat) in an acutely ill patient. It is an important part of intensive care medicine, anesthesiology, trauma surgery and emergency medicine. W ...
area, commonly referred to as "Trauma" or "Resus", is a key area in most departments. The most seriously ill or injured patients will be dealt with in this area, as it contains the equipment and staff required for dealing with immediately life-threatening illnesses and injuries. In such situations, the time in which the patient is treated is crucial. Typical resuscitation staffing involves at least one attending physician, and at least one and usually two nurses with trauma and Advanced Cardiac Life Support training. These personnel may be assigned to the resuscitation area for the entirety of the shift or may be "on call" for resuscitation coverage (i.e. if a critical case presents via walk-in triage or ambulance, the team will be paged to the resuscitation area to deal with the case immediately). Resuscitation cases may also be attended by residents, radiographers, ambulance personnel, respiratory therapists, hospital pharmacists and students of any of these professions depending upon the skill mix needed for any given case and whether or not the hospital provides teaching services.
Patients who exhibit signs of being seriously ill but are not in immediate danger of life or limb will be triaged to "acute care" or "majors", where they will be seen by a physician and receive a more thorough assessment and treatment. Examples of "majors" include chest pain, difficulty breathing, abdominal pain and neurological complaints. Advanced diagnostic testing may be conducted at this stage, including laboratory testing of blood and/or urine, ultrasonography, CT or MRI scanning. Medications appropriate to manage the patient's condition will also be given. Depending on underlying causes of the patient's chief complaint, he or she may be discharged home from this area or admitted to the hospital for further treatment.
Patients whose condition is not immediately life-threatening will be sent to an area suitable to deal with them, and these areas might typically be termed as a ''prompt care'' or ''minors'' area. Such patients may still have been found to have significant problems, including fractures, dislocations, and lacerations requiring suturing
A surgical suture, also known as a stitch or stitches, is a medical device used to hold body tissues together and approximate wound edges after an injury or surgery. Application generally involves using a needle with an attached length of threa ...
.
Children can present particular challenges in treatment. Some departments have dedicated pediatrics
Pediatrics ( also spelled ''paediatrics'' or ''pædiatrics'') is the branch of medicine that involves the medical care of infants, children, adolescents, and young adults. In the United Kingdom, paediatrics covers many of their youth until th ...
areas, and some departments employ a play therapist whose job is to put children at ease to reduce the anxiety caused by visiting the emergency department, as well as provide distraction therapy for simple procedures.
Many hospitals have a separate area for evaluation of psychiatric problems. These are often staffed by psychiatrist
A psychiatrist is a physician who specializes in psychiatry, the branch of medicine devoted to the diagnosis, prevention, study, and treatment of mental disorders. Psychiatrists are physicians and evaluate patients to determine whether their sy ...
s and mental health nurses and social worker
Social work is an academic discipline and practice-based profession concerned with meeting the basic needs of individuals, families, groups, communities, and society as a whole to enhance their individual and collective well-being. Social work ...
s. There is typically at least one room for people who are actively a risk to themselves or others (e.g. suicidal).
Fast decisions on life-and-death cases are critical in hospital emergency departments. As a result, doctors face great pressures to overtest and overtreat. The fear of missing something often leads to extra blood tests and imaging scans for what may be harmless chest pains, run-of-the-mill head bumps, and non-threatening stomach aches, with a high cost on the health care system.
Nomenclature in English
''Emergency department'' became commonly used when emergency medicine was recognized as a medical specialty, and hospitals and medical centres developed departments of emergency medicine to provide services. Other common variations include 'emergency ward,' 'emergency centre' or 'emergency unit'. ''Accident and emergency (A&E)'' is deprecated in the United Kingdom but still in common parlance. It is also still in use in Hong Kong. Earlier terms such as 'casualty' or 'casualty department' were previously used officially and continue to be used informally. The same applies to 'emergency room,' 'emerg,' or 'ER' in North America, originating when emergency facilities were provided in a single room of the hospital by the department of surgery.Signage
Regardless of naming convention, there is a widespread usage of directional signage in white text on a red background across the world, which indicates the location of the emergency department, or a hospital with such facilities. Signs on emergency departments may contain additional information. In some American states, there is close regulation of the design and content of such signs. For example, California requires wording such as "Comprehensive Emergency Medical Service" and "Physician On Duty", to prevent persons in need of critical care from presenting to facilities that are not fully equipped and staffed. In some countries, including the United States and Canada, a smaller facility that may provide assistance in medical emergencies is known as a clinic. Larger communities often have walk-in clinics where people with medical problems that would not be considered serious enough to warrant an emergency department visit can be seen. These clinics often do not operate on a 24-hour basis. Very large clinics may operate as "free-standing emergency centres", which are open 24 hours and can manage a very large number of conditions. However, if a patient presents to a free-standing clinic with a condition requiring hospital admission, he or she must be transferred to an actual hospital, as these facilities do not have the capability to provide inpatient care.Santa Clara Valley Medical Center
Santa Clara Valley Medical Center, commonly known as Valley Medical Center or simply Valley Medical, is a prominent 731-bed public tertiary, teaching, and research hospital in San Jose, California. Located in the Fruitdale neighborhood of Wes ...
File:Ed st marys hospital rochester.JPG, Mayo Clinic Hospital in Rochester
File:Kliniek Sint-Jan spoedgevallen.jpg, Trilingual signage in French, Dutch and English at an emergency department in Brussels, Belgium
United States
TheCenters for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services (CMS), is a federal agency within the United States Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer M ...
(CMS) classified emergency departments into two types: Type A, the majority, which are open 24 hours a day, 7 days a week, 365 days a year; and those who are not, Type B. Many US emergency departments are exceedingly busy. A study found that in 2009, there were an estimated 128,885,040 ED encounters in US hospitals. Approximately one-fifth of ED visits in 2010 were for patients under the age of 18 years. In 2009–2010, a total of 19.6 million emergency department visits in the United States were made by persons aged 65 and over. Most encounters (82.8 percent) resulted in treatment and release; 17.2 percent were admitted to inpatient care.
The 1986 Emergency Medical Treatment and Active Labor Act is an act of the United States Congress, that requires emergency departments, if the associated hospital receives payments from Medicare, to provide appropriate medical examination and emergency treatment to all individuals seeking treatment for a medical condition, regardless of citizenship, legal status, or ability to pay. Like an unfunded mandate, there are no reimbursement provisions.
Rates of ED visits rose between 2006 and 2011 for almost every patient characteristic and location. The total rate of ED visits increased 4.5% in that time. However, the rate of visits for patients under one year of age declined 8.3%.
A survey of New York area doctors in February 2007 found that injuries and even deaths have been caused by excessive waits for hospital beds by ED patients. A 2005 patient survey found an average ED wait time from 2.3 hours in Iowa to 5.0 hours in Arizona.
One inspection of Los Angeles area hospitals by Congressional staff found the EDs operating at an average of 116% of capacity (meaning there were more patients than available treatment spaces) with insufficient beds to accommodate victims of a terrorist attack the size of the 2004 Madrid train bombings
The 2004 Madrid train bombings (also known in Spain as 11M) were a series of coordinated, nearly simultaneous bombings against the Cercanías Madrid, Cercanías commuter train system of Madrid, Spain, on the morning of 11 March 2004—three days ...
. Three of the five Level I trauma centres were on "diversion," meaning ambulances with all but the most severely injured patients were being directed elsewhere because the ED could not safely accommodate any more patients. This controversial practice was banned in Massachusetts (except for major incidents, such as a fire in the ED), effective 1 January 2009; in response, hospitals have devoted more staff to the ED at peak times and moved some elective procedures to non-peak times.
In 2009, there were 1,800 EDs in the country. In 2011, about 421 out of every 1,000 people in the United States visited the emergency department; five times as many were discharged as were admitted. Rural areas are the highest rate of ED visits (502 per 1,000 population) and large metro counties had the lowest (319 visits per 1,000 population). By region, the Midwest had the highest rate of ED visits (460 per 1,000 population) and Western States had the lowest (321 visits per 1,000 population).
Freestanding
In addition to the normal hospital based emergency departments a trend has developed in some states (including Texas and Colorado) of emergency departments not attached to hospitals. These new emergency departments are referred to as free standing emergency departments. The rationale for these operations is the ability to operate outside of hospital policies that may lead to increased wait times and reduced patient satisfaction. These departments have attracted controversy due to consumer confusion around their prices and insurance coverage. In 2017, the largest operator, Adeptus Health, declared bankruptcy.Overuse and utilization management
Patients may visit the emergency room for non-emergencies, which typically costs the patient and themanaged care
The term managed care or managed healthcare is used in the United States to describe a group of activities intended to reduce the cost of providing health care and providing American health insurance while improving the quality of that care ("man ...
insurance company more, and therefore the insurance company may apply utilization management to deny coverage. In 2004, a study found that emergency room visits were the most common reason for appealing disputes over coverage after receiving service. In 2017, Anthem
An anthem is a musical composition of celebration, usually used as a symbol for a distinct group, particularly the national anthems of countries. Originally, and in music theory and religious contexts, it also refers more particularly to short ...
expanded this denial coverage more broadly, provoking public policy reactions.
United Kingdom

Critical conditions handled
Cardiac arrest
Cardiac arrest may occur in the ED/A&E or a patient may be transported by ambulance to the emergency department already in this state. Treatment is basiclife support
Life support comprises the treatments and techniques performed in an emergency in order to support life after the failure of one or more vital organs. Healthcare providers and emergency medical technicians are generally certified to perform basic ...
and advanced life support as taught in advanced life support
Life support comprises the treatments and techniques performed in an emergency in order to support life after the failure of one or more vital organs. Healthcare providers and emergency medical technicians are generally certified to perform basic ...
and advanced cardiac life support courses.
Heart attack
Patients arriving to the emergency department with a myocardial infarction (heart attack) are likely to be triaged to the resuscitation area. They will receive oxygen and monitoring and have an early ECG; aspirin will be given if not contraindicated or not already administered by the ambulance team; morphine or diamorphine will be given for pain; sub lingual (under the tongue) or buccal (between cheek and upper gum) glyceryl trinitrate (nitroglycerin
Nitroglycerin (NG), (alternative spelling of nitroglycerine) also known as trinitroglycerin (TNG), nitro, glyceryl trinitrate (GTN), or 1,2,3-trinitroxypropane, is a dense, colorless, oily, explosive liquid most commonly produced by nitrating g ...
) (GTN or NTG) will be given, unless contraindicated by the presence of other drugs.
An ECG that reveals ST segment elevation suggests complete blockage of one of the main coronary arteries. These patients require immediate reperfusion (re-opening) of the occluded vessel. This can be achieved in two ways: thrombolysis (clot-busting medication) or percutaneous transluminal coronary angioplasty (PTCA). Both of these are effective in reducing significantly the mortality of myocardial infarction. Many centers are now moving to the use of PTCA as it is somewhat more effective than thrombolysis if it can be administered early. This may involve transfer to a nearby facility with facilities for angioplasty.
Trauma
Major trauma, the term for patients with multiple injuries, often from a motor vehicle crash or a major fall, is initially handled in the Emergency Department. However, trauma is a separate (surgical) specialty from emergency medicine (which is itself a medical specialty, and has certifications in the United States from the American Board of Emergency Medicine). Trauma is treated by a trauma team who have been trained using the principles taught in the internationally recognized Advanced Trauma Life Support (ATLS) course of theAmerican College of Surgeons
The American College of Surgeons is an educational association of surgeons created in 1913.American College of Surgeons Online "What is the American College of Surgeons?"/ref>
See also
*American College of Physicians
The American College o ...
. Some other international training bodies have started to run similar courses based on the same principles.
The services that are provided in an emergency department can range from x-rays and the setting of broken bones to those of a full-scale trauma centre. A patient's chance of survival is greatly improved if the patient receives definitive treatment (i.e. surgery or reperfusion) within one hour of an accident (such as a car accident) or onset of acute illness (such as a heart attack). This critical time frame is commonly known as the " golden hour".
Some emergency departments in smaller hospitals are located near a helipad which is used by helicopters to transport a patient to a trauma centre. This inter-hospital transfer is often done when a patient requires advanced medical care unavailable at the local facility. In such cases the emergency department can only stabilize
Stabilizer, stabiliser, stabilisation or stabilization may refer to:
Chemistry and food processing
* Stabilizer (chemistry), a substance added to prevent unwanted change in state of another substance
** Polymer stabilizers are stabilizers use ...
the patient for transport.
Mental illness
Some patients arrive at an emergency department for a complaint of mental illness. In many jurisdictions (including many U.S. states), patients who appear to be mentally ill and to present a danger to themselves or others may be brought against their will to an emergency department by law enforcement officers for psychiatric examination. The emergency department conducts medical clearance rather than treats acute behavioral disorders. From the emergency department, patients with significant mental illness may be transferred to a psychiatric unit (in many cases involuntarily). In recent years, EmPATH units have been developed to relieve pressure on hospital emergency departments and improve the treatment of psychiatric emergencies. Emergency departments are often the first point of contact with healthcare for people whoself-harm
Self-harm is intentional behavior that is considered harmful to oneself. This is most commonly regarded as direct injury of one's own skin tissues usually without a suicidal intention. Other terms such as cutting, self-injury and self-mutilatio ...
. As such they are crucial in supporting them and can play a role in preventing suicide. At the same time, according to a study conducted in England, people who self-harm often experience that they don't receive meaningful care at the emergency department.
Asthma and COPD
Acute exacerbations of chronic respiratory diseases, mainly asthma and chronic obstructive pulmonary disease (COPD), are assessed as emergencies and treated withoxygen therapy
Oxygen therapy, also known as supplemental oxygen, is the use of oxygen as medical treatment. Acute indications for therapy include hypoxemia (low blood oxygen levels), carbon monoxide toxicity and cluster headache. It may also be prophylactica ...
, bronchodilators, steroid
A steroid is a biologically active organic compound with four rings arranged in a specific molecular configuration. Steroids have two principal biological functions: as important components of cell membranes that alter membrane fluidity; and a ...
s or theophylline, have an urgent chest X-ray
A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in med ...
and arterial blood gases and are referred for intensive care if necessary. Noninvasive ventilation in the ED has reduced the requirement for tracheal intubation in many cases of severe exacerbations of COPD.
Special facilities, training, and equipment
An ED requires different equipment and different approaches than most other hospital divisions. Patients frequently arrive with unstable conditions, and so must be treated quickly. They may be unconscious, and information such as their medical history, allergies, and blood type may be unavailable. ED staff are trained to work quickly and effectively even with minimal information. ED staff must also interact efficiently with pre-hospital care providers such as EMTs, paramedics, and others who are occasionally based in an ED. The pre-hospital providers may use equipment unfamiliar to the average physician, but ED physicians must be expert in using (and safely removing) specialized equipment, since devices such as military anti-shock trousers ("MAST") and traction splints require special procedures. Among other reasons, given that they must be able to handle specialized equipment, physicians can now specialize in emergency medicine, and EDs employ many such specialists. ED staff have much in common with ambulance and fire crews, combat medics,search and rescue
Search and rescue (SAR) is the search for and provision of aid to people who are in distress or imminent danger. The general field of search and rescue includes many specialty sub-fields, typically determined by the type of terrain the search ...
teams, and disaster response teams. Often, joint training and practice drills are organized to improve the coordination of this complex response system. Busy EDs exchange a great deal of equipment with ambulance crews, and both must provide for replacing, returning, or reimbursing for costly items.
Cardiac arrest and major trauma are relatively common in EDs, so defibrillators, automatic ventilation and CPR machines, and bleeding control dressings are used heavily. Survival in such cases is greatly enhanced by shortening the wait for key interventions, and in recent years some of this specialized equipment has spread to pre-hospital settings. The best-known example is defibrillators, which spread first to ambulances, then in an automatic version to police cars and fire apparatus, and most recently to public spaces such as airports, office buildings, hotels, and even shopping malls.
Because time is such an essential factor in emergency treatment, EDs typically have their own diagnostic equipment to avoid waiting for equipment installed elsewhere in the hospital. Nearly all have radiographic examination rooms staffed by dedicated Radiographer, and many now have full radiology facilities including CT scanners and ultrasonography equipment. Laboratory services may be handled on a priority basis by the hospital lab, or the ED may have its own "STAT Lab" for basic labs (blood counts, blood typing, toxicology screens, etc.) that must be returned very rapidly.
Non-emergency use
Metrics applicable to the ED can be grouped into three main categories, volume, cycle time, and patient satisfaction. Volume metrics including arrivals per hour, percentage of ED beds occupied, and age of patients are understood at a basic level at all hospitals as an indication for staffing requirements. Cycle time metrics are the mainstays of the evaluation and tracking of process efficiency and are less widespread since an active effort is needed to collect and analyze this data. Patient satisfaction metrics, already commonly collected by nursing groups, physician groups, and hospitals, are useful in demonstrating the impact of changes in patient perception of care over time. Since patient satisfaction metrics are derivative and subjective, they are less useful in primary process improvement. Health information exchanges can reduce nonurgent ED visits by supplying current data about admissions, discharges, and transfers to health plans and accountable care organizations, allowing them to shift ED use to primary care settings. In allprimary care trust
Primary care trusts (PCTs) were part of the National Health Service in England from 2001 to 2013. PCTs were largely administrative bodies, responsible for commissioning primary, community and secondary health services from providers. Until 31 May ...
s there are out of hours medical consultations provided by general practitioners or nurse practitioners.
In the United States, high costs are incurred by non-emergency use of the emergency room. The National Hospital Ambulatory Medical Care Survey looked at the ten most common symptoms for which giving rise to emergency room visits (cough, sore throat, back pain, fever, headache, abdominal pain, chest pain, other pain, shortness of breath, vomiting) and made suggestions as to which would be the most cost-effective choice among virtual care, retail clinic
A walk-in clinic (also known as a walk-in centre) is a medical facility that accepts patients on a walk-in basis and with no appointment required. A number of Health professional, healthcare service providers fall under the walk-in clinic umbrell ...
, urgent care, or emergency room
An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of pati ...
. Notably, certain complaints may also be addressed by a telephone call to a person's primary care provider.
In the United States, and many other countries, hospitals are beginning to create areas in their emergency rooms for people with minor injuries. These are commonly referred as ''Fast Track'' or ''Minor Care'' units. These units are for people with non-life-threatening injuries. The use of these units within a department have been shown to significantly improve the flow of patients through a department and to reduce waiting times. Urgent care clinics are another alternative, where patients can go to receive immediate care for non-life-threatening conditions. To reduce the strain on limited ED resources, American Medical Response created a checklist that allows EMTs to identify intoxicated individuals who can be safely sent to detoxification facilities instead.
Overcrowding
Emergency department overcrowding is when function of a department is hindered by an inability to treat all patients in an adequate manner. This is a common occurrence in emergency departments worldwide. Overcrowding causes inadequate patient care which leads to poorer patient outcomes. To address this problem, escalation policies are used by emergency departments when responding to an increase in demand (e.g., a sudden inflow of patients) or a reduction in capacity (e.g., a lack of beds to admit patients). The policies aim to maintain the ability to deliver patient care, without compromising safety, by modifying "normal" processes.Emergency department waiting times
Emergency department (ED) waiting times have a serious impact on patient mortality, morbidity with readmission in less than 30 days, length of stay, and patient satisfaction. The probability of death increases each 3 minutes for 1% in case of major injuries in the abdomen part. (Journal of Trauma and Acute Care Surgery) Equipment in emergency departments follows the prompt treatment principle with the least possible patient transfers from admittance to X-ray diagnostics. A review of the literature bears out the logical premise that since the outcome of treatment for all diseases and injuries is time-sensitive, the sooner treatment is rendered, the better the outcome. Various studies reported significant associations between waiting times and higher mortality and morbidity among those who survived. It is clear from the literature that untimely hospital deaths and morbidity can be reduced by reductions in ED waiting times.Exit block
While a significant proportion of people attending emergency departments are discharged home after treatment, many require admission for ongoing observation or treatment, or to ensure adequate social care before discharge is possible. If people requiring admission are not able to be moved to inpatient beds swiftly, "exit block" or "access block" occurs. This often leads to crowding and impairs flow to the point that it can lead to delays in appropriate treatment for newly presenting cases ("arrival access block"). This phenomenon is more common in densely populated areas, and affects pediatric departments less than adults ones. Exit block can lead to delays in care both in the people awaiting inpatient beds ("boarding") and those who newly present to an exit blocked department. Various solutions have been proposed, such as changes in staffing or increasing inpatient capacity.Frequent flyers
Frequent flyers are persons who will present themselves at a hospital multiple times, usually those with complex medical requirements or with psychological issues complicating medical management. These persons contribute to overcrowding and typically require more hospital resources although they do not account for a significant number of visits. To help prevent inappropriate emergency department use and return visits, some hospitals offer care coordination and support services such as at-home and in-shelter transitional primary care for frequent flyers and short-term housing for homeless patients recovering after discharge.The role of telemedicine
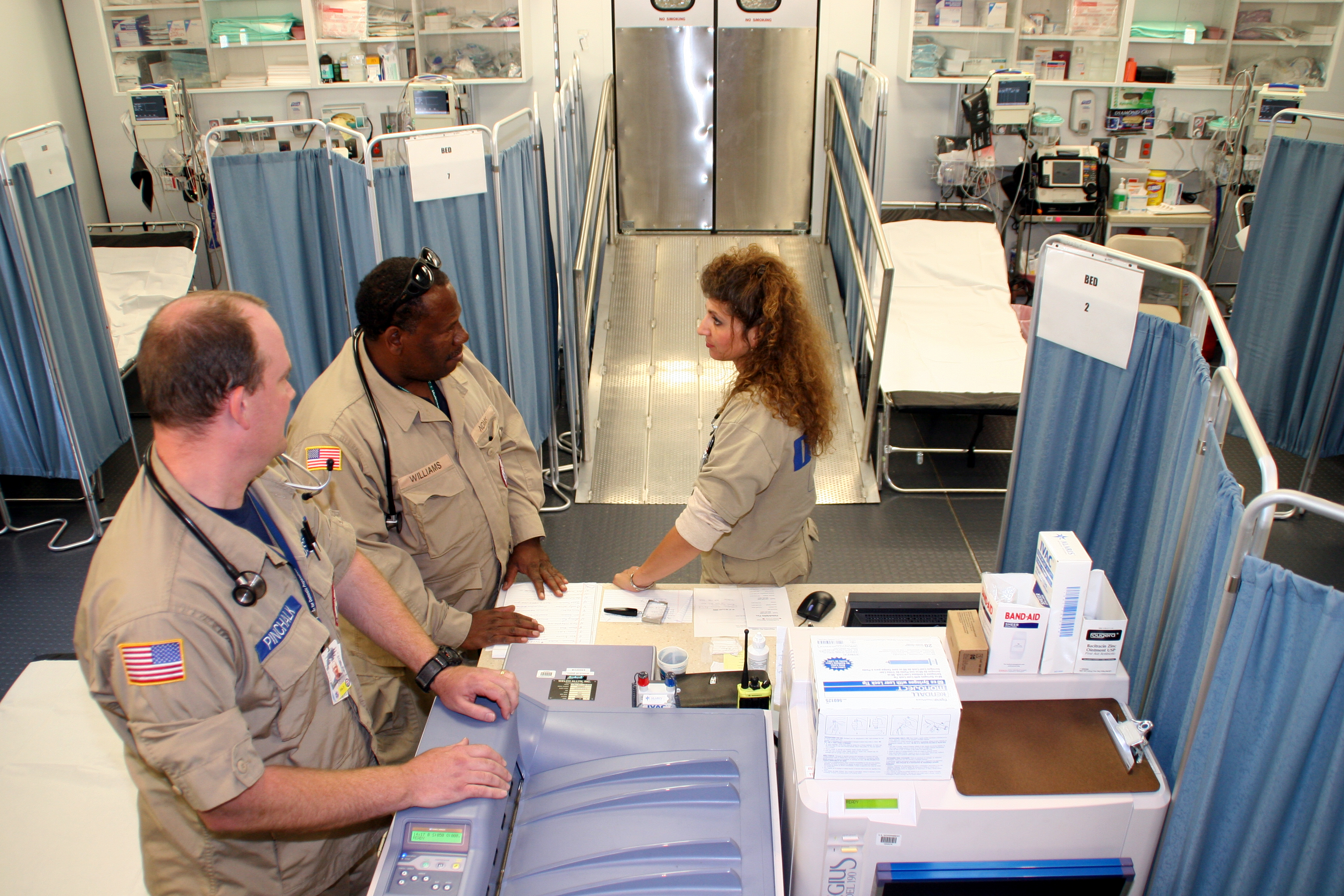
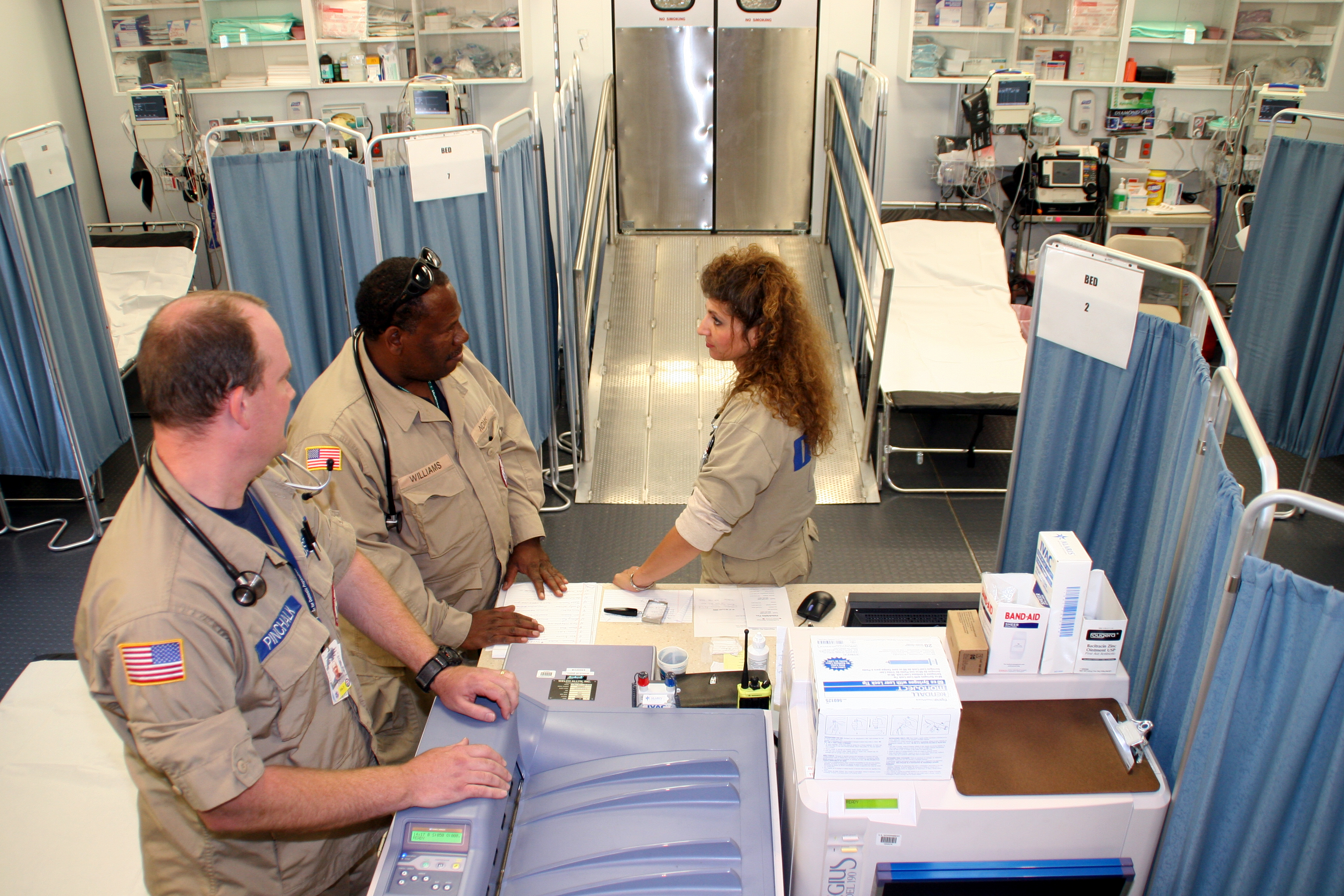
One study found that the implementation of telemedicine services in Saudi Arabia showed to be effective in reducing emergency department overload by providing medical advices to less- and non-urgent patients and deal with their minor medical issues.In the military
Emergency departments in the military benefit from the added support of enlisted personnel who are capable of performing a wide variety of tasks they have been trained for through specialized military schooling. For example, in United States Military Hospitals, Air Force Aerospace Medical Technicians and Navy Hospital Corpsmen perform tasks that fall under the scope of practice of both doctors (i.e. sutures, staples and incision and drainages) and nurses (i.e. medication administration, foley catheter insertion, and obtaining intravenous access) and also perform splinting of injured extremities, nasogastric tube insertion, intubation, wound cauterizing, eye irrigation, and much more. Often, some civilian education and/or certification will be required such as an EMT certification, in case of the need to provide care outside the base where the member is stationed. The presence of highly trained enlisted personnel in an Emergency Departments drastically reduces the workload on nurses and doctors.Violence against healthcare workers
According to a survey at an urban inner-city tertiary care centre in Vancouver, 57% of health care workers were physically assaulted in 1996. 73% were afraid of patients as a result of violence, 49% hid their identities from patients, 74% had reduced job satisfaction. Over one-quarter of the respondents took days off because of violence. Of respondents no longer working in the emergency department, 67% reported that they had left the job at least partly owing to violence. Twenty-four-hour security and a workshop on violence prevention strategies were felt to be the most useful potential interventions. Physical exercise, sleep and the company of family and friends were the most frequent coping strategies cited by those surveyed.Medication errors
 Medication errors are issues that lead to incorrect medication distribution or potential for patient harm. As of 2014, around 3% of all hospital-related adverse effects were due to medication errors in the emergency department (ED); between 4% and 14% of medications given to patients in the ED were incorrect and children were particularly at risk.
Errors can arise if the doctor prescribes the wrong medication, if the prescription intended by the doctor is not the one actually communicated to the
Medication errors are issues that lead to incorrect medication distribution or potential for patient harm. As of 2014, around 3% of all hospital-related adverse effects were due to medication errors in the emergency department (ED); between 4% and 14% of medications given to patients in the ED were incorrect and children were particularly at risk.
Errors can arise if the doctor prescribes the wrong medication, if the prescription intended by the doctor is not the one actually communicated to the pharmacy
Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medicines. It is a miscellaneous science as it links heal ...
due to an illegibly-written prescription or misheard verbal order, if the pharmacy dispenses the wrong medication, or if the medication is then given to the wrong person.
The ED is a riskier environment than other areas of the hospital due to medical practitioners not knowing the patient as well as they know longer term hospital patients, due to time pressure caused by overcrowding, and due to the emergency-driven nature of the medicine that is practiced there.
See also
* Acute Assessment Unit * Emergency department in France * Emergency medical services * Morgue * Walk-in clinicReferences
Further reading
* *External links
ED visits
(US) (National Center for Health Statistics)
Academic Emergency Medicine
, , Elsvier
Physicians on Call: California's Patchwork Approach to Emergency Department Coverage
Wait Time for Treatment in Hospital Emergency Departments, 2009.
Hyattsville, Md.:
U.S. Department of Health and Human Services
The United States Department of Health and Human Services (HHS) is a cabinet-level executive branch department of the U.S. federal government created to protect the health of all Americans and providing essential human services. Its motto is " ...
, Centers for Disease Control and Prevention, National Center for Health Statistics
The National Center for Health Statistics (NCHS) is a U.S. government agency that provides statistical information to guide actions and policies to improve the public health of the American people. It is a unit of the Centers for Disease Control ...
, 2012.
{{Authority control
Emergency medicine
Hospital departments