Diabetes (other) on:
[Wikipedia]
[Google]
[Amazon]
Diabetes, also known as diabetes mellitus, is a group of
 The classic symptoms of untreated diabetes are unintended weight loss, polyuria (increased urination), polydipsia (increased thirst), and polyphagia (increased hunger). Symptoms may develop rapidly (weeks or months) in type 1 diabetes, while they usually develop much more slowly and may be subtle or absent in type 2 diabetes.
Several other signs and symptoms can mark the onset of diabetes although they are Symptom#Types, not specific to the disease. In addition to the known symptoms listed above, they include blurred vision, headache, fatigue (medical), fatigue, slow Wound healing, healing of cuts, and Pruritus, itchy skin. Prolonged high blood glucose can cause glucose absorption in the Lens (anatomy), lens of the eye, which leads to changes in its shape, resulting in vision changes. Long-term vision loss can also be caused by diabetic retinopathy. A number of skin rashes that can occur in diabetes are collectively known as diabetic dermadromes.
The classic symptoms of untreated diabetes are unintended weight loss, polyuria (increased urination), polydipsia (increased thirst), and polyphagia (increased hunger). Symptoms may develop rapidly (weeks or months) in type 1 diabetes, while they usually develop much more slowly and may be subtle or absent in type 2 diabetes.
Several other signs and symptoms can mark the onset of diabetes although they are Symptom#Types, not specific to the disease. In addition to the known symptoms listed above, they include blurred vision, headache, fatigue (medical), fatigue, slow Wound healing, healing of cuts, and Pruritus, itchy skin. Prolonged high blood glucose can cause glucose absorption in the Lens (anatomy), lens of the eye, which leads to changes in its shape, resulting in vision changes. Long-term vision loss can also be caused by diabetic retinopathy. A number of skin rashes that can occur in diabetes are collectively known as diabetic dermadromes.
 All forms of diabetes increase the risk of long-term complications. These typically develop after many years (10–20) but may be the first symptom in those who have otherwise not received a diagnosis before that time.
The major long-term complications relate to damage to blood vessels. Diabetes doubles the risk of
All forms of diabetes increase the risk of long-term complications. These typically develop after many years (10–20) but may be the first symptom in those who have otherwise not received a diagnosis before that time.
The major long-term complications relate to damage to blood vessels. Diabetes doubles the risk of
 Type 1 diabetes is partly Genetic disorder, inherited, with multiple genes, including certain Human leukocyte antigen, HLA genotypes, known to influence the risk of diabetes. In genetically susceptible people, the onset of diabetes can be triggered by one or more environmental factors, such as a viral infection or diet. Several viruses have been implicated, but to date there is no stringent evidence to support this hypothesis in humans. Among dietary factors, data suggest that gliadin (a protein present in gluten) may play a role in the development of type 1 diabetes, but the mechanism is not fully understood.
Type 1 diabetes can occur at any age, and a significant proportion is diagnosed during adulthood. Latent autoimmune diabetes of adults (LADA) is the diagnostic term applied when type 1 diabetes develops in adults; it has a slower onset than the same condition in children. Given this difference, some use the unofficial term "type 1.5 diabetes" for this condition. Adults with LADA are frequently initially misdiagnosed as having type 2 diabetes, based on age rather than a cause.
Type 1 diabetes is partly Genetic disorder, inherited, with multiple genes, including certain Human leukocyte antigen, HLA genotypes, known to influence the risk of diabetes. In genetically susceptible people, the onset of diabetes can be triggered by one or more environmental factors, such as a viral infection or diet. Several viruses have been implicated, but to date there is no stringent evidence to support this hypothesis in humans. Among dietary factors, data suggest that gliadin (a protein present in gluten) may play a role in the development of type 1 diabetes, but the mechanism is not fully understood.
Type 1 diabetes can occur at any age, and a significant proportion is diagnosed during adulthood. Latent autoimmune diabetes of adults (LADA) is the diagnostic term applied when type 1 diabetes develops in adults; it has a slower onset than the same condition in children. Given this difference, some use the unofficial term "type 1.5 diabetes" for this condition. Adults with LADA are frequently initially misdiagnosed as having type 2 diabetes, based on age rather than a cause.
 Type 2 diabetes is characterized by
Type 2 diabetes is characterized by
 Insulin is the principal hormone that regulates the uptake of
Insulin is the principal hormone that regulates the uptake of
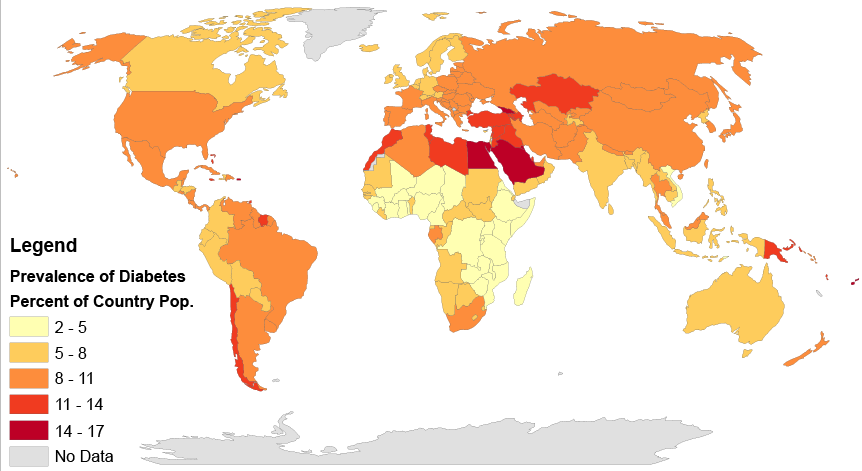
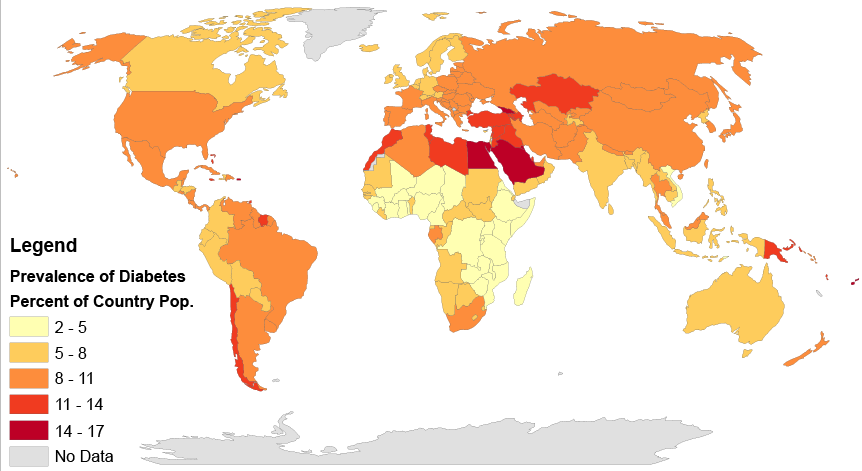
 In 2017, 425 million people had diabetes worldwide, up from an estimated 382 million people in 2013 and from 108 million in 1980. Accounting for the shifting age structure of the global population, the prevalence of diabetes is 8.8% among adults, nearly double the rate of 4.7% in 1980. Type 2 makes up about 90% of the cases. Some data indicate rates are roughly equal in women and men, but male excess in diabetes has been found in many populations with higher type 2 incidence, possibly due to sex-related differences in insulin sensitivity, consequences of obesity and regional body fat deposition, and other contributing factors such as high blood pressure, tobacco smoking, and alcohol intake.
The WHO estimates that diabetes resulted in 1.5 million deaths in 2012, making it the 8th leading cause of death. However another 2.2 million deaths worldwide were attributable to high blood glucose and the increased risks of cardiovascular disease and other associated complications (e.g. kidney failure), which often lead to premature death and are often listed as the underlying cause on death certificates rather than diabetes. For example, in 2017, the International Diabetes Federation (IDF) estimated that diabetes resulted in 4.0 million deaths worldwide, using modeling to estimate the total number of deaths that could be directly or indirectly attributed to diabetes.
Diabetes occurs throughout the world but is more common (especially type 2) in more developed countries. The greatest increase in rates has however been seen in low- and middle-income countries, where more than 80% of diabetic deaths occur. The fastest prevalence increase is expected to occur in Asia and Africa, where most people with diabetes will probably live in 2030. The increase in rates in developing countries follows the trend of urbanization and lifestyle changes, including increasingly sedentary lifestyles, less physically demanding work and the global nutrition transition, marked by increased intake of foods that are high energy-dense but nutrient-poor (often high in sugar and saturated fats, sometimes referred to as the "Western-style" diet). The global number of diabetes cases might increase by 48% between 2017 and 2045.
As of 2020, 38% of all US adults had prediabetes. Prediabetes is an early stage of diabetes.
In 2017, 425 million people had diabetes worldwide, up from an estimated 382 million people in 2013 and from 108 million in 1980. Accounting for the shifting age structure of the global population, the prevalence of diabetes is 8.8% among adults, nearly double the rate of 4.7% in 1980. Type 2 makes up about 90% of the cases. Some data indicate rates are roughly equal in women and men, but male excess in diabetes has been found in many populations with higher type 2 incidence, possibly due to sex-related differences in insulin sensitivity, consequences of obesity and regional body fat deposition, and other contributing factors such as high blood pressure, tobacco smoking, and alcohol intake.
The WHO estimates that diabetes resulted in 1.5 million deaths in 2012, making it the 8th leading cause of death. However another 2.2 million deaths worldwide were attributable to high blood glucose and the increased risks of cardiovascular disease and other associated complications (e.g. kidney failure), which often lead to premature death and are often listed as the underlying cause on death certificates rather than diabetes. For example, in 2017, the International Diabetes Federation (IDF) estimated that diabetes resulted in 4.0 million deaths worldwide, using modeling to estimate the total number of deaths that could be directly or indirectly attributed to diabetes.
Diabetes occurs throughout the world but is more common (especially type 2) in more developed countries. The greatest increase in rates has however been seen in low- and middle-income countries, where more than 80% of diabetic deaths occur. The fastest prevalence increase is expected to occur in Asia and Africa, where most people with diabetes will probably live in 2030. The increase in rates in developing countries follows the trend of urbanization and lifestyle changes, including increasingly sedentary lifestyles, less physically demanding work and the global nutrition transition, marked by increased intake of foods that are high energy-dense but nutrient-poor (often high in sugar and saturated fats, sometimes referred to as the "Western-style" diet). The global number of diabetes cases might increase by 48% between 2017 and 2045.
As of 2020, 38% of all US adults had prediabetes. Prediabetes is an early stage of diabetes.
American Diabetes Association
IDF Diabetes Atlas
National Diabetes Education Program
ADA's Standards of Medical Care in Diabetes 2019
* * {{DEFAULTSORT:Diabetes Mellitus Diabetes, Wikipedia medicine articles ready to translate Metabolic disorders Wikipedia emergency medicine articles ready to translate Endocrine diseases Cardiovascular diseases Disability by type
metabolic disorder
A metabolic disorder is a disorder that negatively alters the body's processing and distribution of macronutrients, such as proteins, fats, and carbohydrates. Metabolic disorders can happen when abnormal chemical reactions in the body alter the ...
s characterized by a high blood sugar level (hyperglycemia
Hyperglycemia is a condition in which an excessive amount of glucose circulates in the blood plasma. This is generally a blood sugar level higher than 11.1 mmol/L (200 mg/dL), but symptoms may not start to become noticeable until even ...
) over a prolonged period of time. Symptoms often include frequent urination
Frequent urination, or urinary frequency (sometimes called pollakiuria), is the need to urinate more often than usual. Diuretics are medications that increase urinary frequency. Nocturia is the need of frequent urination at night. The most common c ...
, increased thirst and increased appetite. If left untreated, diabetes leads to many health complications. Acute
Acute may refer to:
Science and technology
* Acute angle
** Acute triangle
** Acute, a leaf shape in the glossary of leaf morphology
* Acute (medicine), a disease that it is of short duration and of recent onset.
** Acute toxicity, the adverse eff ...
complications can include diabetic ketoacidosis, hyperosmolar hyperglycemic state, or death
Death is the irreversible cessation of all biological functions that sustain an organism. For organisms with a brain, death can also be defined as the irreversible cessation of functioning of the whole brain, including brainstem, and brain ...
. Serious long-term complications include cardiovascular disease
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, h ...
, stroke
A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functionin ...
, chronic kidney disease
Chronic kidney disease (CKD) is a type of kidney disease in which a gradual loss of kidney function occurs over a period of months to years. Initially generally no symptoms are seen, but later symptoms may include leg swelling, feeling tired, vo ...
, foot ulcers
The foot ( : feet) is an anatomical structure found in many vertebrates. It is the terminal portion of a limb which bears weight and allows locomotion. In many animals with feet, the foot is a separate organ at the terminal part of the leg made ...
, damage to the nerves, damage to the eyes, and cognitive impairment.
Diabetes is due to either the pancreas
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e. it has both an end ...
not producing enough insulin
Insulin (, from Latin ''insula'', 'island') is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the ''INS'' gene. It is considered to be the main anabolic hormone of the body. It regulates the metabolism o ...
, or the cells of the body not responding properly to the insulin produced. Insulin is a hormone which is responsible for helping glucose
Glucose is a simple sugar with the molecular formula . Glucose is overall the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, using ...
from food get into cells to be used for energy. There are three main types of diabetes mellitus:
* Type 1 diabetes
Type 1 diabetes (T1D), formerly known as juvenile diabetes, is an autoimmune disease that originates when cells that make insulin (beta cells) are destroyed by the immune system. Insulin is a hormone required for the cells to use blood sugar for ...
results from failure of the pancreas to produce enough insulin due to loss of beta cell
Beta cells (β-cells) are a type of cell found in pancreatic islets that synthesize and secrete insulin and amylin. Beta cells make up 50–70% of the cells in human islets. In patients with Type 1 diabetes, beta-cell mass and function are dimini ...
s. This form was previously referred to as "insulin-dependent diabetes mellitus" or "juvenile diabetes". The loss of beta cells is caused by an autoimmune response. The cause of this autoimmune response is unknown. Although Type 1 diabetes usually appears during childhood or adolescence, it can also develop in adults.
* Type 2 diabetes
Type 2 diabetes, formerly known as adult-onset diabetes, is a form of diabetes mellitus that is characterized by high blood sugar, insulin resistance, and relative lack of insulin. Common symptoms include increased thirst, frequent urination, ...
begins with insulin resistance
Insulin resistance (IR) is a pathological condition in which cell (biology), cells fail to respond normally to the hormone insulin.
Insulin is a hormone that facilitates the transport of glucose from blood into cells, thereby reducing blood gluco ...
, a condition in which cells fail to respond to insulin properly. As the disease progresses, a lack of insulin may also develop. This form was previously referred to as "non insulin-dependent diabetes mellitus" or "adult-onset diabetes". Type 2 diabetes is more common in older adults, but a significant increase in the prevalence of obesity among children has led to more cases of type 2 diabetes in younger people. The most common cause is a combination of excessive body weight and insufficient exercise.
* Gestational diabetes
Gestational diabetes is a condition in which a woman without diabetes develops high blood sugar levels during pregnancy. Gestational diabetes generally results in few symptoms; however, it increases the risk of pre-eclampsia, depression, and of ...
is the third main form, and occurs when Pregnancy, pregnant women without a previous history of diabetes develop high blood sugar levels. In women with gestational diabetes, blood sugar usually returns to normal soon after delivery. However, women who had gestational diabetes during pregnancy have a higher risk of developing type 2 diabetes later in life.
Type 1 diabetes must be managed with Insulin injection (soluble), insulin injections. Prevention and treatment of type 2 diabetes involves maintaining a healthy diet, regular physical exercise, a normal body weight, and avoiding Tobacco use, use of tobacco. Type 2 diabetes may be treated with oral antidiabetic Oral antidiabetic, medications, with or without insulin. Control of blood pressure and maintaining proper foot and eye care are important for people with the disease. Insulin and some oral medications can cause hypoglycemia, low blood sugar (hypoglycemia). Bariatric surgery, Weight loss surgery in those with obesity is sometimes an effective measure in those with type 2 diabetes. Gestational diabetes usually resolves after the birth of the baby.
, an estimated 463 million people had diabetes worldwide (8.8% of the adult population), with type 2 diabetes making up about 90% of the cases. Rates are similar in women and men. Trends suggest that rates will continue to rise. Diabetes at least doubles a person's risk of early death. In 2019, diabetes resulted in approximately 4.2 million deaths. It is the 7th leading cause of death globally. The global economic cost of diabetes-related health expenditure in 2017 was estimated at billion. In the United States, diabetes cost nearly US$327 billion in 2017. Average medical expenditures among people with diabetes are about 2.3 times higher.
Signs and symptoms
Diabetic emergencies
People with diabetes (usually but not exclusively in type 1 diabetes) may also experience diabetic ketoacidosis (DKA), a metabolic disturbance characterized by nausea, vomiting and abdominal pain, the smell of acetone on the breath, deep breathing known as Kussmaul breathing, and in severe cases a decreased level of consciousness. DKA requires emergency treatment in hospital. A rarer but more dangerous condition is hyperosmolar hyperglycemic state (HHS), which is more common in type 2 diabetes and is mainly the result of dehydration caused by high blood sugars. Treatment-related Hypoglycemia, low blood sugar (hypoglycemia) is common in people with type 1 and also type 2 diabetes depending on the medication being used. Most cases are mild and are not considered Medical emergency, medical emergencies. Effects can range from Anxiety, feelings of unease, Perspiration, sweating, Tremor, trembling, and increased appetite in mild cases to more serious effects such as Altered mental status, confusion, changes in behavior such as Aggression, aggressiveness, Epileptic seizure, seizures, unconsciousness, and rarely permanent brain damage ordeath
Death is the irreversible cessation of all biological functions that sustain an organism. For organisms with a brain, death can also be defined as the irreversible cessation of functioning of the whole brain, including brainstem, and brain ...
in severe cases. Tachypnea, Rapid breathing, sweating, and cold, pale skin are characteristic of low blood sugar but not definitive. Mild to moderate cases are self-treated by eating or drinking something high in rapidly absorbed carbohydrates. Severe cases can lead to unconsciousness and must be treated with intravenous glucose or Glucagon rescue, injections with glucagon.
Complications
 All forms of diabetes increase the risk of long-term complications. These typically develop after many years (10–20) but may be the first symptom in those who have otherwise not received a diagnosis before that time.
The major long-term complications relate to damage to blood vessels. Diabetes doubles the risk of
All forms of diabetes increase the risk of long-term complications. These typically develop after many years (10–20) but may be the first symptom in those who have otherwise not received a diagnosis before that time.
The major long-term complications relate to damage to blood vessels. Diabetes doubles the risk of cardiovascular disease
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, h ...
and about 75% of deaths in people with diabetes are due to coronary artery disease. Other macrovascular diseases include stroke
A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functionin ...
, and peripheral artery disease. These complications are also a strong risk factor for severe COVID-19 illness.
The primary complications of diabetes due to damage in small blood vessels include damage to the eyes, kidneys, and nerves. Damage to the eyes, known as diabetic retinopathy, is caused by damage to the blood vessels in the retina of the eye, and can result in gradual vision loss and eventual Visual impairment, blindness. Diabetes also increases the risk of having glaucoma, cataracts, and other eye problems. It is recommended that people with diabetes visit an Ophthalmologist, eye doctor once a year. Damage to the kidneys, known as diabetic nephropathy, can lead to Glomerulosclerosis, tissue scarring, Proteinuria, urine protein loss, and eventually chronic kidney disease, sometimes requiring Kidney dialysis, dialysis or kidney transplantation. Damage to the nerves of the body, known as diabetic neuropathy, is the most common complication of diabetes. The symptoms can include Hypoesthesia, numbness, Paresthesia, tingling, Sudomotor, sudomotor dysfunction, pain, and altered pain sensation, which can lead to damage to the skin. diabetic foot, Diabetes-related foot problems (such as diabetic foot ulcers) may occur, and can be difficult to treat, occasionally requiring amputation. Additionally, proximal diabetic neuropathy causes painful muscle atrophy and Muscle weakness, weakness.
There is a link between cognitive deficit and diabetes. Compared to those without diabetes, those with the disease have a 1.2 to 1.5-fold greater rate of decline in cognitive function. Having diabetes, especially when on insulin, increases the risk of falls in older people.
Causes
Diabetes mellitus is classified into six categories: type 1 diabetes, type 2 diabetes, hybrid forms of diabetes, hyperglycemia first detected during pregnancy, "unclassified diabetes", and "other specific types". "Hybrid forms of diabetes" include Latent autoimmune diabetes of adults, slowly evolving, immune-mediated diabetes of adults and Ketosis-prone diabetes, ketosis-prone type 2 diabetes. "Hyperglycemia first detected during pregnancy" includes gestational diabetes mellitus and diabetes mellitus in pregnancy (type 1 or type 2 diabetes first diagnosed during pregnancy). The "other specific types" are a collection of a few dozen individual causes. Diabetes is a more variable disease than once thought and people may have combinations of forms.Type 1
Type 1 diabetes is characterized by loss of the insulin-producingbeta cell
Beta cells (β-cells) are a type of cell found in pancreatic islets that synthesize and secrete insulin and amylin. Beta cells make up 50–70% of the cells in human islets. In patients with Type 1 diabetes, beta-cell mass and function are dimini ...
s of the pancreatic islets, leading to insulin deficiency. This type can be further classified as immune-mediated or Idiopathic disease, idiopathic. The majority of type 1 diabetes is of an immune-mediated nature, in which a T cell-mediated autoimmunity, autoimmune attack leads to the loss of beta cells and thus insulin. It causes approximately 10% of diabetes mellitus cases in North America and Europe. Most affected people are otherwise healthy and of a healthy weight when onset occurs. Sensitivity and responsiveness to insulin are usually normal, especially in the early stages. Although it has been called "juvenile diabetes" due to the frequent onset in children, the majority of individuals living with type 1 diabetes are now adults.
"Brittle" diabetes, also known as unstable diabetes or labile diabetes, is a term that was traditionally used to describe the dramatic and recurrent swings in glucose
Glucose is a simple sugar with the molecular formula . Glucose is overall the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, using ...
levels, often occurring for no apparent reason in insulin-dependent diabetes. This term, however, has no biologic basis and should not be used. Still, type 1 diabetes can be accompanied by irregular and unpredictable high blood sugar levels, and the potential for diabetic ketoacidosis or serious low blood sugar levels. Other complications include an impaired counterregulatory response to low blood sugar, infection, gastroparesis (which leads to erratic absorption of dietary carbohydrates), and endocrinopathies (e.g., Addison's disease). These phenomena are believed to occur no more frequently than in 1% to 2% of persons with type 1 diabetes.
 Type 1 diabetes is partly Genetic disorder, inherited, with multiple genes, including certain Human leukocyte antigen, HLA genotypes, known to influence the risk of diabetes. In genetically susceptible people, the onset of diabetes can be triggered by one or more environmental factors, such as a viral infection or diet. Several viruses have been implicated, but to date there is no stringent evidence to support this hypothesis in humans. Among dietary factors, data suggest that gliadin (a protein present in gluten) may play a role in the development of type 1 diabetes, but the mechanism is not fully understood.
Type 1 diabetes can occur at any age, and a significant proportion is diagnosed during adulthood. Latent autoimmune diabetes of adults (LADA) is the diagnostic term applied when type 1 diabetes develops in adults; it has a slower onset than the same condition in children. Given this difference, some use the unofficial term "type 1.5 diabetes" for this condition. Adults with LADA are frequently initially misdiagnosed as having type 2 diabetes, based on age rather than a cause.
Type 1 diabetes is partly Genetic disorder, inherited, with multiple genes, including certain Human leukocyte antigen, HLA genotypes, known to influence the risk of diabetes. In genetically susceptible people, the onset of diabetes can be triggered by one or more environmental factors, such as a viral infection or diet. Several viruses have been implicated, but to date there is no stringent evidence to support this hypothesis in humans. Among dietary factors, data suggest that gliadin (a protein present in gluten) may play a role in the development of type 1 diabetes, but the mechanism is not fully understood.
Type 1 diabetes can occur at any age, and a significant proportion is diagnosed during adulthood. Latent autoimmune diabetes of adults (LADA) is the diagnostic term applied when type 1 diabetes develops in adults; it has a slower onset than the same condition in children. Given this difference, some use the unofficial term "type 1.5 diabetes" for this condition. Adults with LADA are frequently initially misdiagnosed as having type 2 diabetes, based on age rather than a cause.
Type 2
 Type 2 diabetes is characterized by
Type 2 diabetes is characterized by insulin resistance
Insulin resistance (IR) is a pathological condition in which cell (biology), cells fail to respond normally to the hormone insulin.
Insulin is a hormone that facilitates the transport of glucose from blood into cells, thereby reducing blood gluco ...
, which may be combined with relatively reduced insulin secretion. The defective responsiveness of body tissues to insulin is believed to involve the insulin receptor. However, the specific defects are not known. Diabetes mellitus cases due to a known defect are classified separately. Type 2 diabetes is the most common type of diabetes mellitus accounting for 95% of diabetes. Many people with type 2 diabetes have evidence of prediabetes (impaired fasting glucose and/or impaired glucose tolerance) before meeting the criteria for type 2 diabetes. The progression of prediabetes to overt type 2 diabetes can be slowed or reversed by lifestyle changes or Anti-diabetic drug, medications that improve insulin sensitivity or reduce the Glycogenolysis, liver's glucose production.
Type 2 diabetes is primarily due to lifestyle factors and genetics. A number of lifestyle factors are known to be important to the development of type 2 diabetes, including obesity (defined by a body mass index of greater than 30), lack of physical activity, poor Diet (nutrition), diet, stress (biology), stress, and urbanization. Excess body fat is associated with 30% of cases in people of Chinese and Japanese descent, 60–80% of cases in those of European and African descent, and 100% of Pima Indians and Pacific Islanders. Even those who are not obese may have a high waist–hip ratio.
Dietary factors such as sugar-sweetened drinks are associated with an increased risk. The type of fats in the diet is also important, with saturated fat and trans fats increasing the risk and polyunsaturated fat, polyunsaturated and monounsaturated fat decreasing the risk. Eating white rice excessively may increase the risk of diabetes, especially in Chinese and Japanese people. Lack of physical activity may increase the risk of diabetes in some people.
Adverse Childhood Experiences Study, Adverse childhood experiences, including abuse, neglect, and household difficulties, increase the likelihood of type 2 diabetes later in life by 32%, with neglect having the strongest effect.
Antipsychotic, Antipsychotic medication side effects (specifically metabolic abnormalities, dyslipidemia and weight gain) and unhealthy lifestyles (including poor diet and decreased physical activity), are potential risk factors.
Gestational diabetes
Gestational diabetes resembles type 2 diabetes in several respects, involving a combination of relatively inadequate insulin secretion and responsiveness. It occurs in about 2–10% of all pregnancy, pregnancies and may improve or disappear after delivery. It is recommended that all pregnant women get tested starting around 24–28 weeks gestation. It is most often diagnosed in the second or third trimester because of the increase in insulin-antagonist hormone levels that occurs at this time. However, after pregnancy approximately 5–10% of women with gestational diabetes are found to have another form of diabetes, most commonly type 2. Gestational diabetes is fully treatable, but requires careful medical supervision throughout the pregnancy. Management may include dietary changes, blood glucose monitoring, and in some cases, insulin may be required. Though it may be transient, untreated gestational diabetes can damage the health of the fetus or mother. Risks to the baby include macrosomia (high birth weight), Congenital heart defect, congenital heart and central nervous system abnormalities, and skeletal muscle malformations. Increased levels of insulin in a fetus's blood may inhibit fetal surfactant production and cause infant respiratory distress syndrome. A Bilirubin#Hyperbilirubinemia, high blood bilirubin level may result from hemolysis, red blood cell destruction. In severe cases, perinatal death may occur, most commonly as a result of poor placental perfusion due to vascular impairment. Labor induction may be indicated with decreased placental function. A caesarean section may be performed if there is marked fetal distress or an increased risk of injury associated with macrosomia, such as shoulder dystocia.Other types
Maturity onset diabetes of the young (MODY) is a rare Dominance (genetics), autosomal dominant inherited form of diabetes, due to one of several single-gene mutations causing defects in insulin production. It is significantly less common than the three main types, constituting 1–2% of all cases. The name of this disease refers to early hypotheses as to its nature. Being due to a defective gene, this disease varies in age at presentation and in severity according to the specific gene defect; thus, there are at least 13 subtypes of MODY. People with MODY often can control it without using insulin. Some cases of diabetes are caused by the body's tissue receptors not responding to insulin (even when insulin levels are normal, which is what separates it from type 2 diabetes); this form is very uncommon. Genetic mutations (Dominance (genetics), autosomal or Mitochondrion, mitochondrial) can lead to defects in beta cell function. Abnormal insulin action may also have been genetically determined in some cases. Any disease that causes extensive damage to the pancreas may lead to diabetes (for example, chronic pancreatitis and cystic fibrosis). Diseases associated with excessive secretion of insulin receptor, insulin-antagonistic hormones can cause diabetes (which is typically resolved once the hormone excess is removed). Many drugs impair insulin secretion and some toxins damage pancreatic beta cells, whereas others increaseinsulin resistance
Insulin resistance (IR) is a pathological condition in which cell (biology), cells fail to respond normally to the hormone insulin.
Insulin is a hormone that facilitates the transport of glucose from blood into cells, thereby reducing blood gluco ...
(especially glucocorticoids which can provoke "steroid diabetes"). The ICD-10 (1992) diagnostic entity, ''malnutrition-related diabetes mellitus'' (ICD-10 code E12), was deprecated by the World Health Organization (WHO) when the current taxonomy was introduced in 1999.
Yet another form of diabetes that people may develop is double diabetes. This is when a type 1 diabetic becomes insulin resistant, the hallmark for type 2 diabetes or has a family history for type 2 diabetes. It was first discovered in 1990 or 1991.
The following is a list of disorders that may increase the risk of diabetes:Unless otherwise specified, reference is: Table 20-5 in
* Genetic defects of β-cell function
** Maturity onset diabetes of the young
** Mitochondrial DNA mutations
* Genetic defects in insulin processing or insulin action
** Defects in proinsulin conversion
** Insulin gene mutations
** Insulin receptor mutations
* Exocrine pancreatic defects (see Type 3c diabetes, i.e. pancreatogenic diabetes)
** Chronic pancreatitis
** Pancreatectomy
** Pancreatic neoplasia
** Cystic fibrosis
** Hemochromatosis
** Fibrocalculous pancreatopathy
* Endocrinopathies
** Growth hormone excess (acromegaly)
** Cushing syndrome
** Hyperthyroidism
** Hypothyroidism
** Pheochromocytoma
** Glucagonoma
* Infections
** Cytomegalovirus infection
** Coxsackie B4 virus, Coxsackievirus B
* Drugs
** Glucocorticoids
** Thyroid hormone
** β-adrenergic agonists
** Statins
Pathophysiology
 Insulin is the principal hormone that regulates the uptake of
Insulin is the principal hormone that regulates the uptake of glucose
Glucose is a simple sugar with the molecular formula . Glucose is overall the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, using ...
from the blood into most cells of the body, especially liver, adipose tissue and muscle, except smooth muscle, in which insulin acts via the IGF-1. Therefore, deficiency of insulin or the insensitivity of its Receptor (biochemistry), receptors play a central role in all forms of diabetes mellitus.
The body obtains glucose from three main sources: the intestinal absorption of food; the breakdown of glycogen (glycogenolysis), the storage form of glucose found in the liver; and gluconeogenesis, the generation of glucose from non-carbohydrate substrates in the body. Insulin plays a critical role in regulating glucose levels in the body. Insulin can inhibit the breakdown of glycogen or the process of gluconeogenesis, it can stimulate the transport of glucose into fat and muscle cells, and it can stimulate the storage of glucose in the form of glycogen.
Insulin is released into the blood by beta cells (β-cells), found in the islets of Langerhans in the pancreas, in response to rising levels of blood glucose, typically after eating. Insulin is used by about two-thirds of the body's cells to absorb glucose from the blood for use as fuel, for conversion to other needed molecules, or for storage. Lower glucose levels result in decreased insulin release from the beta cells and in the breakdown of glycogen to glucose. This process is mainly controlled by the hormone glucagon, which acts in the opposite manner to insulin.
If the amount of insulin available is insufficient, or if cells respond poorly to the effects of insulin (insulin resistance
Insulin resistance (IR) is a pathological condition in which cell (biology), cells fail to respond normally to the hormone insulin.
Insulin is a hormone that facilitates the transport of glucose from blood into cells, thereby reducing blood gluco ...
), or if the insulin itself is defective, then glucose is not absorbed properly by the body cells that require it, and is not stored appropriately in the liver and muscles. The net effect is persistently high levels of blood glucose, poor Protein biosynthesis, protein synthesis, and other metabolic derangements, such as metabolic acidosis in cases of complete insulin deficiency.
When glucose concentration in the blood remains high over time, the kidneys reach a threshold of reabsorption, and the body excretes glucose in the urine (glycosuria). This increases the osmotic pressure of the urine and inhibits reabsorption of water by the kidney, resulting in increased urine production (polyuria) and increased fluid loss. Lost blood volume is replaced osmotically from water in body cells and other body compartments, causing dehydration and increased thirst (polydipsia). In addition, intracellular glucose deficiency stimulates appetite leading to excessive food intake (polyphagia).
Diagnosis
Diabetes mellitus is diagnosed with a test for the glucose content in the blood, and is diagnosed by demonstrating any one of the following: * Fasting glucose, Fasting plasma glucose level ≥ 7.0 mmol/L (126 mg/dL). For this test, blood is taken after a period of fasting, i.e. in the morning before breakfast, after the patient had sufficient time to fast overnight. * Plasma glucose ≥ 11.1 mmol/L (200 mg/dL) two hours after a 75 gram oral glucose load as in a glucose tolerance test (OGTT) * Symptoms of high blood sugar and plasma glucose ≥ 11.1 mmol/L (200 mg/dL) either while fasting or not fasting * Glycated hemoglobin (HbA1C) ≥ 48 mmol/mol (≥ 6.5 Diabetes control and complications trial, DCCT %). A positive result, in the absence of unequivocal high blood sugar, should be confirmed by a repeat of any of the above methods on a different day. It is preferable to measure a fasting glucose level because of the ease of measurement and the considerable time commitment of formal glucose tolerance testing, which takes two hours to complete and offers no prognostic advantage over the fasting test. According to the current definition, two fasting glucose measurements above 7.0 mmol/L (126 mg/dL) is considered diagnostic for diabetes mellitus. Per the WHO, people with fasting glucose levels from 6.1 to 6.9 mmol/L (110 to 125 mg/dL) are considered to have impaired fasting glycemia, impaired fasting glucose. People with plasma glucose at or above 7.8 mmol/L (140 mg/dL), but not over 11.1 mmol/L (200 mg/dL), two hours after a 75 gram oral glucose load are considered to have impaired glucose tolerance. Of these two prediabetic states, the latter in particular is a major risk factor for progression to full-blown diabetes mellitus, as well as cardiovascular disease. The American Diabetes Association (ADA) since 2003 uses a slightly different range for impaired fasting glucose of 5.6 to 6.9 mmol/L (100 to 125 mg/dL). Glycated hemoglobin is better than fasting glucose for determining risks of cardiovascular disease and death from any cause.Prevention
There is no known Preventive healthcare, preventive measure for type 1 diabetes. Type 2 diabetes—which accounts for 85–90% of all cases worldwide—can often be prevented or delayed by maintaining a normal body weight, engaging in physical activity, and eating a healthy diet. Higher levels of physical activity (more than 90 minutes per day) reduce the risk of diabetes by 28%. Dietary changes known to be effective in helping to prevent diabetes include maintaining a diet rich in whole grains and Dietary fiber, fiber, and choosing good fats, such as the polyunsaturated fats found in nuts, vegetable oils, and fish. Limiting sugary beverages and eating less red meat and other sources of saturated fat can also help prevent diabetes. Tobacco smoking is also associated with an increased risk of diabetes and its complications, so smoking cessation can be an important preventive measure as well. The relationship between type 2 diabetes and the main modifiable risk factors (excess weight, unhealthy diet, physical inactivity and tobacco use) is similar in all regions of the world. There is growing evidence that the underlying determinants of diabetes are a reflection of the major forces driving social, economic and cultural change: globalization, urbanization, population aging, and the general health policy environment.Management
Diabetes management concentrates on keeping blood sugar levels as close to normal, without causing low blood sugar. This can usually be accomplished with dietary changes, exercise, weight loss, and use of appropriate medications (insulin, oral medications). Learning about the disease and actively participating in the treatment is important, since complications are far less common and less severe in people who have well-managed blood sugar levels. Per the American College of Physicians, the goal of treatment is an HbA1C level of 7-8%. Attention is also paid to other health problems that may accelerate the negative effects of diabetes. These include tobacco smoking, smoking, hypertension, high blood pressure, metabolic syndrome obesity, and lack of regular exercise. Diabetic shoe, Specialized footwear is widely used to reduce the risk of Diabetic foot ulcer, diabetic foot ulcers by relieving the pressure on the foot. Foot examination for patients living with diabetes should be done annually which includes sensation testing, foot biomechanics, vascular integrity and foot structure. The principles of managing diabetes may be similar across the general population with diabetes, however some considerations may need to be addressed when tailoring intervention, mainly in special populations. Considering those with severe Mental disorder, mental illness, the efficacy of type 2 diabetes self-management interventions is still poorly explored, with insufficient scientific evidence to show whether these interventions have similar results to those observed in general population.Lifestyle
People with diabetes can benefit from education about the disease and treatment, dietary changes, and exercise, with the goal of keeping both short-term and long-term blood glucose levels Diabetes management#Glycemic control, within acceptable bounds. In addition, given the associated higher risks of cardiovascular disease, lifestyle modifications are recommended to control blood pressure. Weight loss can prevent progression from prediabetes to Diabetes mellitus, diabetes type 2, decrease the risk of cardiovascular disease, or result in a partial remission in people with diabetes. No single dietary pattern is best for all people with diabetes. Healthy dietary patterns, such as the Mediterranean diet, low-carbohydrate diet, or DASH diet, are often recommended, although evidence does not support one over the others. According to the ADA, "reducing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia", and for individuals with type 2 diabetes who cannot meet the glycemic targets or where reducing anti-glycemic medications is a priority, low-carbohydrate diet, low or very-low carbohydrate diets are a viable approach. For overweight people with type 2 diabetes, any diet that achieves weight loss is effective.Medications
Glucose control
Most medications used to treat diabetes act by lowering glucose, blood sugar levels through different mechanisms. There is broad consensus that when people with diabetes maintain tight glucose control – keeping the glucose levels in their blood within normal ranges – they experience fewer complications, such as diabetic nephropathy, kidney problems or diabetic retinopathy, eye problems. There is however debate as to whether this is appropriate and cost effective for people later in life in whom the risk of hypoglycemia may be more significant. There are a number of different classes of anti-diabetic medications. Type 1 diabetes requires treatment withinsulin
Insulin (, from Latin ''insula'', 'island') is a peptide hormone produced by beta cells of the pancreatic islets encoded in humans by the ''INS'' gene. It is considered to be the main anabolic hormone of the body. It regulates the metabolism o ...
, ideally using a "basal bolus" regimen that most closely matches normal insulin release: long-acting insulin for the basal rate and short-acting insulin with meals. Type 2 diabetes is generally treated with medication that is taken by mouth (e.g. metformin) although some eventually require injectable treatment with insulin or GLP-1 agonists.
Metformin is generally recommended as a first-line treatment for type 2 diabetes, as there is good evidence that it decreases mortality. It works by decreasing the liver's production of glucose. Several other groups of drugs, mostly given by mouth, may also decrease blood sugar in type 2 diabetes. These include agents that increase insulin release (sulfonylureas), agents that decrease absorption of sugar from the intestines (acarbose), agents that inhibit the enzyme dipeptidyl peptidase-4 (DPP-4) that inactivates incretins such as GLP-1 and GIP (sitagliptin), agents that make the body more sensitive to insulin (thiazolidinedione) and agents that increase the excretion of glucose in the urine (SGLT2 inhibitors). When insulin is used in type 2 diabetes, a long-acting formulation is usually added initially, while continuing oral medications. Doses of insulin are then increased until glucose targets are reached.
Blood pressure lowering
Cardiovascular disease is a serious complication associated with diabetes, and many international guidelines recommend blood pressure treatment targets that are lower than 140/90 mmHg for people with diabetes. However, there is only limited evidence regarding what the lower targets should be. A 2016 systematic review found potential harm to treating to targets lower than 140 mmHg, and a subsequent systematic review in 2019 found no evidence of additional benefit from blood pressure lowering to between 130 – 140mmHg, although there was an increased risk of adverse events. 2015 American Diabetes Association recommendations are that people with diabetes and albuminuria should receive an inhibitor of the renin-angiotensin system to reduce the risks of progression to end-stage renal disease, cardiovascular events, and death. There is some evidence that angiotensin converting enzyme inhibitors (ACEIs) are superior to other inhibitors of the renin-angiotensin system such as angiotensin receptor blockers (ARBs), or aliskiren in preventing cardiovascular disease. Although a more recent review found similar effects of ACEIs and ARBs on major cardiovascular and renal outcomes. There is no evidence that combining ACEIs and ARBs provides additional benefits.Aspirin
The use of aspirin to prevent cardiovascular disease in diabetes is controversial. Aspirin is recommended by some in people at high risk of cardiovascular disease, however routine use of aspirin has not been found to improve outcomes in uncomplicated diabetes. 2015 American Diabetes Association recommendations for aspirin use (based on expert consensus or clinical experience) are that low-dose aspirin use is reasonable in adults with diabetes who are at intermediate risk of cardiovascular disease (10-year cardiovascular disease risk, 5–10%). National guidelines for England and Wales by the National Institute for Health and Care Excellence (NICE) recommend against the use of aspirin in people with type 1 or type 2 diabetes who do not have confirmed cardiovascular disease.Surgery
Bariatric surgery, Weight loss surgery in those with obesity and type 2 diabetes is often an effective measure. Many are able to maintain normal blood sugar levels with little or no medications following surgery and long-term mortality is decreased. There is, however, a short-term mortality risk of less than 1% from the surgery. The body mass index cutoffs for when surgery is appropriate are not yet clear. It is recommended that this option be considered in those who are unable to get both their weight and blood sugar under control. A pancreas transplant is occasionally considered for people with type 1 diabetes who have severe complications of their disease, including Chronic kidney disease, end stage kidney disease requiring kidney transplantation.Self-management and support
In countries using a general practitioner system, such as the United Kingdom, care may take place mainly outside hospitals, with hospital-based specialist care used only in case of complications, difficult blood sugar control, or research projects. In other circumstances, general practitioners and specialists share care in a team approach. Home telehealth support can be an effective management technique. The use of technology to deliver educational programs for adults with type 2 diabetes includes computer-based self-management interventions to collect for tailored responses to facilitate self-management. There is no adequate evidence to support effects on cholesterol, blood pressure, Behavior change (public health), behavioral change (such as physical activity levels and dietary), Depression (mood), depression, weight and Quality of life (healthcare), health-related quality of life, nor in other biological, cognitive or emotional outcomes.Epidemiology
History
Diabetes was one of the first diseases described, with an Ancient Egypt, Egyptian manuscript from 1500 Common Era, BCE mentioning "too great emptying of the urine." The Ebers papyrus includes a recommendation for a drink to take in such cases. The first described cases are believed to have been type 1 diabetes. Indian physicians around the same time identified the disease and classified it as ''madhumeha'' or "honey urine", noting the urine would attract ants. The term "diabetes" or "to pass through" was first used in 230 BCE by the Greek Apollonius (physician), Apollonius of Memphis. The disease was considered rare during the time of the Roman empire, with Galen commenting he had only seen two cases during his career. This is possibly due to the diet and lifestyle of the ancients, or because the clinical symptoms were observed during the advanced stage of the disease. Galen named the disease "diarrhea of the urine" (diarrhea urinosa). The earliest surviving work with a detailed reference to diabetes is that of Aretaeus of Cappadocia (2nd or early 3rdcentury CE). He described the symptoms and the course of the disease, which he attributed to the moisture and coldness, reflecting the beliefs of the "Pneumatic school, Pneumatic School". He hypothesized a correlation between diabetes and other diseases, and he discussed differential diagnosis from the snakebite, which also provokes excessive thirst. His work remained unknown in the West until 1552, when the first Latin edition was published in Venice. Two types of diabetes were identified as separate conditions for the first time by the Indian physicians Sushruta and Charaka in 400–500 CE with one type being associated with youth and another type with being overweight. Effective treatment was not developed until the early part of the 20th century when Canadians Frederick Banting and Charles Herbert Best isolated and purified insulin in 1921 and 1922. This was followed by the development of the long-acting insulin NPH insulin, NPH in the 1940s.Etymology
The word ''diabetes'' ( or ) comes from Latin ''diabētēs'', which in turn comes from Ancient Greek διαβήτης (''diabētēs''), which literally means "a passer through; a siphon".Oxford English Dictionary. ''diabetes''. Retrieved 2011-06-10. Ancient Greece, Ancient Greek physician Aretaeus of Cappadocia (Floruit, fl. 1stcentury Common Era, CE) used that word, with the intended meaning "excessive discharge of urine", as the name for the disease. Ultimately, the word comes from Greek διαβαίνειν (''diabainein''), meaning "to pass through", which is composed of δια- (''dia''-), meaning "through" and βαίνειν (''bainein''), meaning "to go". The word "diabetes" is first recorded in English, in the form ''diabete'', in a medical text written around 1425. The word ''wikt:mellitus, mellitus'' ( or ) comes from the classical Latin word ''mellītus'', meaning "mellite"Oxford English Dictionary. ''mellite''. Retrieved 2011-06-10. (i.e. sweetened with honey; honey-sweet). The Latin word comes from ''mell''-, which comes from ''mel'', meaning "honey"; sweetness; pleasant thing, and the suffix -''ītus'', whose meaning is the same as that of the English suffix "-ite".Oxford English Dictionary. ''-ite''. Retrieved 2011-06-10. It was Thomas Willis who in 1675 added "mellitus" to the word "diabetes" as a designation for the disease, when he noticed the urine of a person with diabetes had a sweet taste (glycosuria). This sweet taste had been noticed in urine by the ancient Greeks, Chinese, Egyptians, Indians, and Persian people, Persians .Society and culture
The 1989 "St. Vincent Declaration" was the result of international efforts to improve the care accorded to those with diabetes. Doing so is important not only in terms of quality of life and life expectancy but also economicallyexpenses due to diabetes have been shown to be a major drain on healthand productivity-related resources for healthcare systems and governments. Several countries established more and less successful national diabetes programmes to improve treatment of the disease. People with diabetes who have neuropathic symptoms such as numbness or tingling in feet or hands are twice as likely to be unemployed as those without the symptoms. In 2010, diabetes-related emergency room (ER) visit rates in the United States were higher among people from the lowest income communities (526 per 10,000 population) than from the highest income communities (236 per 10,000 population). Approximately 9.4% of diabetes-related ER visits were for the uninsured.Naming
The term "type 1 diabetes" has replaced several former terms, including childhood-onset diabetes, juvenile diabetes, and insulin-dependent diabetes mellitus. Likewise, the term "type 2 diabetes" has replaced several former terms, including adult-onset diabetes, obesity-related diabetes, and noninsulin-dependent diabetes mellitus. Beyond these two types, there is no agreed-upon standard nomenclature. Diabetes mellitus is also occasionally known as "sugar diabetes" to differentiate it from diabetes insipidus.Other animals
Diabetes can occur in mammals or reptiles. Birds do not develop diabetes because of their unusually high tolerance for elevated blood glucose levels. In animals, diabetes is most commonly encountered in dogs and cats. Middle-aged animals are most commonly affected. Female dogs are twice as likely to be affected as males, while according to some sources, male cats are more prone than females. In both species, all breeds may be affected, but some small dog breeds are particularly likely to develop diabetes, such as Poodle, Miniature Poodles. Feline diabetes is strikingly similar to human type 2 diabetes. The Burmese cat, Burmese, Russian Blue, Abyssinian cat, Abyssinian, and Norwegian Forest cat, Norwegian Forest cat breeds are at higher risk than other breeds. Overweight cats are also at higher risk. The symptoms may relate to fluid loss and polyuria, but the course may also be insidious. Diabetic animals are more prone to infections. The long-term complications recognized in humans are much rarer in animals. The principles of treatment (weight loss, oral antidiabetics, subcutaneous insulin) and management of emergencies (e.g. ketoacidosis) are similar to those in humans.References
External links
American Diabetes Association
IDF Diabetes Atlas
National Diabetes Education Program
ADA's Standards of Medical Care in Diabetes 2019
* * {{DEFAULTSORT:Diabetes Mellitus Diabetes, Wikipedia medicine articles ready to translate Metabolic disorders Wikipedia emergency medicine articles ready to translate Endocrine diseases Cardiovascular diseases Disability by type