cardiac bypass surgery on:
[Wikipedia]
[Google]
[Amazon]
Coronary artery bypass surgery, also known as coronary artery bypass graft (CABG, pronounced "cabbage") is a surgical procedure to treat 
 Coronary artery disease is caused when
Coronary artery disease is caused when
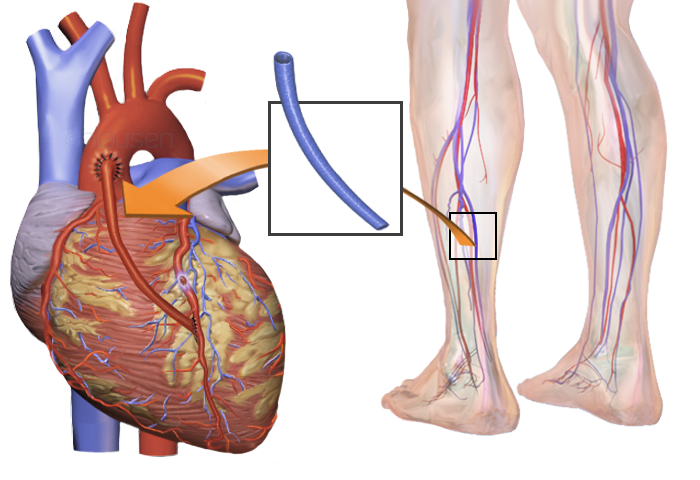
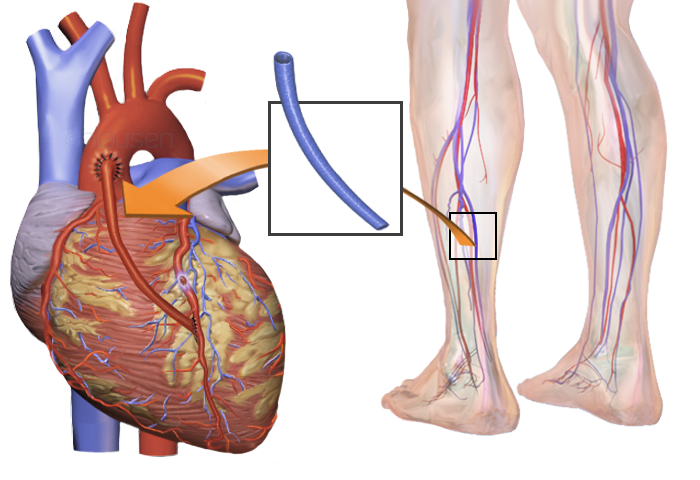
File:Coronary Artery Bypass Surgery.jpg, Coronary Artery Bypass Graft.
File:Coronary Artery Bypass Graft, Single Bypass.jpg, Coronary Artery Bypass Graft, Single Bypass
File:Coronary Artery Bypass Graft, Double Bypass.jpg, Coronary Artery Bypass Graft, Double Bypass.
File:Coronary Artery Bypass Graft, Triple Bypass.jpg, Coronary Artery Bypass Graft, Triple Bypass
File:Coronary Artery Bypass Graft, Quadruple Bypass.jpg, Coronary Artery Bypass Graft, Quadruple Bypass
 Surgical interventions aiming relieve angina and prevent death in the early 20th century, were either sympatheticectomy (a cut on the sympathetic chain that supplies the heart, with disappointing and inconsistent results) or pericardial abrasion (with the hope that adhesions would create significant collateral circulation).French Surgeon
Surgical interventions aiming relieve angina and prevent death in the early 20th century, were either sympatheticectomy (a cut on the sympathetic chain that supplies the heart, with disappointing and inconsistent results) or pericardial abrasion (with the hope that adhesions would create significant collateral circulation).French Surgeon
coronary artery disease
Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of atherosclerotic pla ...
(CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pain
Chest pain is pain or discomfort in the chest, typically the front of the chest. It may be described as sharp, dull, pressure, heaviness or squeezing. Associated symptoms may include pain in the shoulder, arm, upper abdomen, or jaw, along with n ...
caused by CAD, slow the progression of CAD, and increase life expectancy. It aims to bypass narrowings in heart arteries by using arteries or veins harvested from other parts of the body, thus restoring adequate blood supply to the previously ischemic
Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism (to keep tissue alive). Ischemia is generally caused by problems wi ...
(deprived of blood) heart.
There are two main approaches. The first uses a cardiopulmonary bypass machine
Cardiopulmonary bypass (CPB) is a technique in which a machine temporarily takes over the function of the heart and lungs during surgery, maintaining the circulation of blood and oxygen to the body. The CPB pump itself is often referred to as a he ...
, a machine which takes over the functions of the heart and lungs during surgery by circulating blood and oxygen. With the heart in arrest, harvested arteries and veins are used to connect across problematic regions—a construction known as surgical anastomosis
A surgical anastomosis is a surgical technique used to make a new connection between two body structures that carry fluid, such as blood vessels or bowel. For example, an arterial anastomosis is used in vascular bypass and a colonic anastomosis i ...
. In the second approach, called the off-pump coronary artery bypass graft (OPCABG), these anastomoses are constructed while the heart is still beating. The anastomosis supplying the left anterior descending branch is the most significant one and usually, the left internal mammary artery is harvested for use. Other commonly employed sources are the right internal mammary artery, the radial artery
In human anatomy, the radial artery is the main artery of the lateral aspect of the forearm.
Structure
The radial artery arises from the bifurcation of the brachial artery in the antecubital fossa. It runs distally on the anterior part of the f ...
, and the great saphenous vein
The great saphenous vein (GSV, alternately "long saphenous vein"; ) is a large, subcutaneous, superficial vein of the leg. It is the longest vein in the body, running along the length of the lower limb, returning blood from the foot, leg and thig ...
.
Doctors were searching for an effective way to treat chest pain (specifically, angina
Angina, also known as angina pectoris, is chest pain or pressure, usually caused by ischemia, insufficient blood flow to the Cardiac muscle, heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.
Angina is typical ...
, a common symptom of CAD) since the beginning of the 20th century. In the 1960s, CABG was introduced in its modern form and has since become the main treatment for significant CAD. Significant complications of the operation include bleeding, heart problems (heart attack
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may tr ...
, arrhythmia
Arrhythmias, also known as cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults ...
s), stroke
A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functionin ...
, infections (often pneumonia
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity ...
) and injury to the kidneys.

Uses
Coronary artery bypass surgery aims to prevent death fromcoronary artery disease
Coronary artery disease (CAD), also called coronary heart disease (CHD), ischemic heart disease (IHD), myocardial ischemia, or simply heart disease, involves the reduction of blood flow to the heart muscle due to build-up of atherosclerotic pla ...
and improve quality of life by relieving angina
Angina, also known as angina pectoris, is chest pain or pressure, usually caused by ischemia, insufficient blood flow to the Cardiac muscle, heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.
Angina is typical ...
, the associated feeling of chest pain. The decision to perform surgery is informed by studies of CABG's efficacy in various subgroups of cases, based on the lesions' anatomy or how well the heart is functioning. These results are compared with that of other strategies, most importantly percutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
(PCI).
Coronary artery disease
 Coronary artery disease is caused when
Coronary artery disease is caused when coronary arteries
The coronary arteries are the arterial blood vessels of coronary circulation, which transport oxygenated blood to the heart muscle. The heart requires a continuous supply of oxygen to function and survive, much like any other tissue or organ of ...
of the heart accumulate atheromatic plaques, causing stenosis
A stenosis (from Ancient Greek στενός, "narrow") is an abnormal narrowing in a blood vessel or other tubular organ or structure such as foramina and canals. It is also sometimes called a stricture (as in urethral stricture).
''Stricture'' ...
(narrowing) in one or more arteries and risking myocardial infarction
A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may ...
, the interruption of blood supply to the heart. CAD can occur in any of the major vessels of coronary circulation: the left main stem, left ascending artery, circumflex artery, and right coronary artery, and branches thereof. CAD symptoms vary from none, to chest pain when exercising (stable angina), to chest pain even at rest (unstable angina). It can even manifest as a myocardial infarction; if blood flow to the heart is not restored within a few hours, whether spontaneously or by medical intervention, the blood-deprived part of the heart becomes necrotic
Necrosis () is a form of cell injury which results in the premature death of cells in living tissue by autolysis. Necrosis is caused by factors external to the cell or tissue, such as infection, or trauma which result in the unregulated dige ...
(dies) and is scarred. It may lead to other complications such as arrhythmias
Arrhythmias, also known as cardiac arrhythmias, heart arrhythmias, or dysrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults ...
, rupture of the papillary muscles of the heart, or sudden death.
There are various methods of detecting and assessing CAD. Apart from history and clinical examination, noninvasive methods include electrocardiography
Electrocardiography is the process of producing an electrocardiogram (ECG or EKG), a recording of the heart's electrical activity. It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the hear ...
(ECG) at rest or during exercise, and X-ray of the chest. Echocardiography
An echocardiography, echocardiogram, cardiac echo or simply an echo, is an ultrasound of the heart.
It is a type of medical imaging of the heart, using standard ultrasound or Doppler ultrasound.
Echocardiography has become routinely used in t ...
can quantify the functioning of heart tissue by measuring, for example, enlargement of the left ventricle
A ventricle is one of two large chambers toward the bottom of the heart that collect and expel blood towards the peripheral beds within the body and lungs. The blood pumped by a ventricle is supplied by an atrium, an adjacent chamber in the upper ...
, the ejection fraction
An ejection fraction (EF) is the volumetric fraction (or portion of the total) of fluid (usually blood) ejected from a chamber (usually the heart) with each contraction (or heartbeat). It can refer to the cardiac atrium, ventricle, gall bladder, ...
, and the situation of the heart valves
A heart valve is a one-way valve that allows blood to flow in one direction through the chambers of the heart. Four valves are usually present in a mammalian heart and together they determine the pathway of blood flow through the heart. A heart v ...
. The most accurate ways to detect CAD are the coronary angiogram
A coronary catheterization is a minimally invasive procedure to access the coronary circulation and blood filled chambers of the heart using a catheter. It is performed for both diagnostic and interventional (treatment) purposes.
Coronary cathe ...
and the coronary CT angiography
Coronary CT angiography (CTA or CCTA) is the use of computed tomography (CT) angiography to assess the coronary arteries of the heart. The patient receives an intravenous injection of radiocontrast and then the heart is scanned using a high spee ...
. An angiogram can provide detailed anatomy of coronary circulation and lesions. The significance of each lesion is determined by the diameter loss. A diameter loss of 50% translates to a 75% cross-sectional area loss, considered moderate by most groups. Severe stenosis constitutes a diameter loss of 2/3 or more—a >90% loss of cross-sectional area. To more accurately determine the severity of stenosis, interventional cardiologists may also employ intravascular ultrasound
Intravascular ultrasound (IVUS) or intravascular echocardiography is a medical imaging methodology using a specially designed catheter with a miniaturized ultrasound probe attached to the distal end of the catheter. The proximal end of the cath ...
, which can determine the severity and provide information on the composition of the atheromatic plaque. With the technique of fractional flow reserve Fractional flow reserve (FFR) is a diagnostic technique used in coronary catheterization. FFR measures pressure differences across a coronary artery stenosis (narrowing, usually due to atherosclerosis) to determine the likelihood that the stenosis i ...
, the post-stenotic pressure is compared to mean aortic pressure. If the ratio is less than 0.80, then the stenosis is deemed significant.
Indications for CABG
Stable patients
People suffering from angina during exercise are usually first treated with medical therapy. Noninvasive tests (as stress test, nuclear imaging, dobutamine stress echocardiography) help estimate which patients might benefit from undergoing coronary angiography. Generally, when portions of cardiac wall receive less blood than normal, coronary angiography is indicated; then, lesions are identified and inform a decision to undergo PCI or GABG. CABG is generally preferred over PCI when there is a significant burden of plaque on the coronary arteries, that is extensive and complex. Other indicators that a patient will benefit more from CABG rather than PCI include: decreased left-ventricle function; LM disease; and complex triple system disease (including LAD, Cx and RCA), especially when the lesion at LAD is at its proximal part and diabetes.Acute coronary syndrome
During an acute heart event, namedacute coronary syndrome
Acute coronary syndrome (ACS) is a syndrome (a set of signs and symptoms) due to decreased blood flow in the coronary arteries such that part of the heart muscle is unable to function properly or dies. The most common symptom is centrally loca ...
, it is paramount to restore blood flow to heart tissue as fast as possible. Typically, patients arrive at hospital with chest pain. Initially they are treated with medical drugs, particularly the strongest drugs that prevent clots within vessels (dual antiplatelet therapy: aspirin and a P2Y12 inhibitor-like clopidogrel). Patients at risk of ongoing ischemia, undergo PCI and restore blood flow and thus oxygen delivery to the struggling myocardium. In cases where PCI failed to restore blood flow because of anatomic considerations or other technical problems, urgent CABG is indicated to save myocardium. It has also been noted that the timing of the operation, plays a role in survival, it is preferable to delay the surgery if possible (6 hours in cases of nontransmural MI, 3 days in cases of transmural MI)
CABG of coronary lesions is also indicated in mechanical complications of an infarction (ventricular septal defect, papillary muscle rupture or myocardial rupture) should be addressed There are no absolute contraindications of CABG but severe disease of other organs such as liver or brain, limited life expectancy, fragility should be taken into consideration when planning the treatment path of a patient.Other cardiac surgery
CABG is also performed when a patient is to undergo another cardiac surgical procedure, most commonly for valve disease, and at angiography a significant lesion of the coronaries is found. CABG can be employed in other situations other than atheromatic disease of native heart arteries, like for the dissection of coronary arteries (where a rupture of the coronary layers creates a pseudo-lumen and diminishes blood delivery to the heart) caused e.g. by pregnancy, tissue diseases as Enhler-Danlos, Marfan Syndrome, cocaine abuse or Percutaneous Coronary Intervention). A coronary aneurysm is another reason for CABG, for a thrombus might develop within the vessel, and possibly travel further.CABG vs PCI
CABG and percutaneous coronary intervention (PCI) are the two modalities the medical community has to revascularize stenotic lesions of the cardiac arteries. Which one is preferable for each patient is still a matter of debate, but it is clear that in the presence of complex lesions, significant Left Main Disease and in diabetic patients, CABG seems to offer better results to patients than PCI. Strong indications for CABG also include symptomatic patients and in cases where LV function is impaired., CABG offers better results that PCI in left main disease and in multivessel CAD, because of the protection arterial conduits offer to the native arteries of the heart, by producing vasodilator factors and preventing advancement of atherotic plaques. The question which modality has been studied in various trials. Patients with ''unprotected LM Disease'' (runoff of LM is not protected by a patent graft since previous CABG operation) were studied in NOBLE and EXCEL trials. NOBLE, which was published in 2016 is a multi-European country that found that CABG outperforms PCI in the long run (5 years). EXCEL, also published in 2016, found that PCI has similar results to CABG at 3 years, but this similarity fades at 4th year and later (CABG is better to PCI). Diabetic patients were studied in the FREEDOM trial, first published in 2012 and a follow up. It demonstrated a significant advantage in this group of patients when treated with CABG (vs PCI). The superiority was evident in a 3.8 year follow up and, an even further followup at 7.5 years, of the same patients documented again the superiority of CABG, enphasazing the benefits in smokers and younger patients. BEST trial was published in 2015, comparing CABG and the latest technological advancement of PCI, second generation Drug-eluting stents in multivessel disease. Their results were indicative of CABG being a better option for patients with CAD. A trial published in 2021 (Fractional Flow Reserve versus Angiography for Multivessel Evaluation, FAME 3), also concluded that CABG is a safer option than PCI, when comparing results after one year from intervention.Complications
The most common complications of CABG are postoperative bleeding, heart failure, Atrial fibrillation (a form of arrhythmia), stroke, renal dysfunction, and sternal wound infections. Postoperative bleeding occurs in 2-5% of cases and might force the cardiac team to take the patient back to operating theatre to control the bleeding The most common criterion for that is the amount blood drained by chest tubes, left after the operation. Re-operation addresses surgical causes of that bleeding, which might originate from the aorta, the anastomosis or a branch of the conduit insufficiently sealed or from the sternum. Medical causes of bleeding include platelet abnormalities or coagulopathy due to bypass or the rebound heparin effect (heparin administered at the beginning of CPB reappears at blood after its neutralization by protamine). As for heart failure,low cardiac output syndrome
Low or LOW or lows, may refer to:
People
* Low (surname), listing people surnamed Low
Places
* Low, Quebec, Canada
* Low, Utah, United States
* Lo Wu station (MTR code LOW), Hong Kong; a rail station
* Salzburg Airport (ICAO airport code: LO ...
(LCOS) can occur up to 14% of CABG cases and is according to its severity, is treated with inotropes, IABP, optimization of pre- and afterload, or correction of blood gauzes and electrolytes. The aim is to keep a systolic blood pressure above 90mmHg and cardiac index (CI) more than 2.2 L/min/m2. LCOS is often transient. Postoperative Myocardial infarction can occur because of either technical or patients factors- it's incidence is hard to estimate though due to various definitions, but most studies place it between 2 and 10%. New ECG features as Q waves and/or US documented alternation of cardiac wall motions are indicative. Ongoing ischemia might prompt emergency angiography or re-operation. Arrhythmias can also occur, most commonly atrial fibrillation (20-40%) that is treated with correcting electrolyte balance, rate and rhythm control.
Various neurological adverse effects can occur after CABG, with total incidence about 1,5% they can manifest as type 1-focal deficits (such as stroke or coma) or type 2- global ones (such as delirium) . Inflammation caused by CPB, hypoperfusion or cerebral embolism. Cognitive impairment has been reported in up to 80% cases after CABG at discharge and lasting up to 40% for a year. The causes are rather unclear, it seems CPB is not a suspect since even in CABG cases not including CPB (as in Off-Pump CABG), the incidence is the same, whilst PCI has the same incidence of cognitive decline as well.
Infections are also a problem of the postoperative period. Sternal would infections (superficial or deep), most commonly caused by ''Staphylococcus aureus
''Staphylococcus aureus'' is a Gram-positive spherically shaped bacterium, a member of the Bacillota, and is a usual member of the microbiota of the body, frequently found in the upper respiratory tract and on the skin. It is often positive ...
'', can add to mortality. Harvesting of two mammary arteries is a risk factor since the perfusion of sternum is significantly impaired. Pneumonia can also occur. Complications from the GI track have been described, most commonly are caused by peri-operative medications.Procedure
Preoperative workup and strategy
Routine preoperative workup aims to check the baseline status of systems and organs other than heart. Thus a chest x-ray to check lungs, complete blood count, renal and liver function tests are done to screen for abnormalities. Physical examination to determine the quality of the grafts or the safety of removing them, such as varicosities in the legs, or theAllen test
In medicine, Allen's test or the Allen test is a medical sign used in physical examination of arterial blood flow to the hands. It was named for Edgar Van Nuys Allen, who described the original version of the test in 1942.
An altered test, first s ...
in the arm is performed to be sure that blood supply to the arm wont be disturbed critically.
Administration of anticoagulants such as aspirin
Aspirin, also known as acetylsalicylic acid (ASA), is a nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain, fever, and/or inflammation, and as an antithrombotic. Specific inflammatory conditions which aspirin is used to treat inc ...
, clopidogrel
Clopidogrel — sold under the brand name Plavix, among others — is an antiplatelet medication used to reduce the risk of heart disease and stroke in those at high risk. It is also used together with aspirin in heart attacks and following t ...
, ticagrelol
Ticagrelor, sold under the brand name Brilinta among others, is a medication used for the prevention of stroke, heart attack and other events in people with acute coronary syndrome, meaning problems with blood supply in the coronary arteries. ...
and others, is stopped several days before the operation, to prevent excessive bleeding during the operation and in the following period. Warfarin is also stopped for the same reason and the patient starts being administered heparin products after INR falls below 2.0.
After the angiogram is reviewed by the surgical team, targets are selected (that is, which native arteries will be bypassed and where the anastomosis should be placed). Ideally, all major lesions in significant vessels should be addressed. Most commonly, left internal thoracic artery (LITA; formerly, left internal mammary artery, LIMA) is anastomosed to left anterior descending artery (LAD) because the LAD is the most significant artery of the heart, since it supplies a larger portion of myocardium than other arteries.
A conduit can be used to graft one or more native arteries. In the latter case, an end-to-side anastomosis is performed. In the former, utilizing a sequential anastomosis, a graft can then deliver blood to two or more native vessels of the heart. Also, the proximal part of a conduit can be anastomosed to the side of another conduit (by a Y or a T anastomose) adding to the versality of options for the architecture of CABG. It is preferred not to harvest too much length of conduits since it might cause some patients to need re-operation.
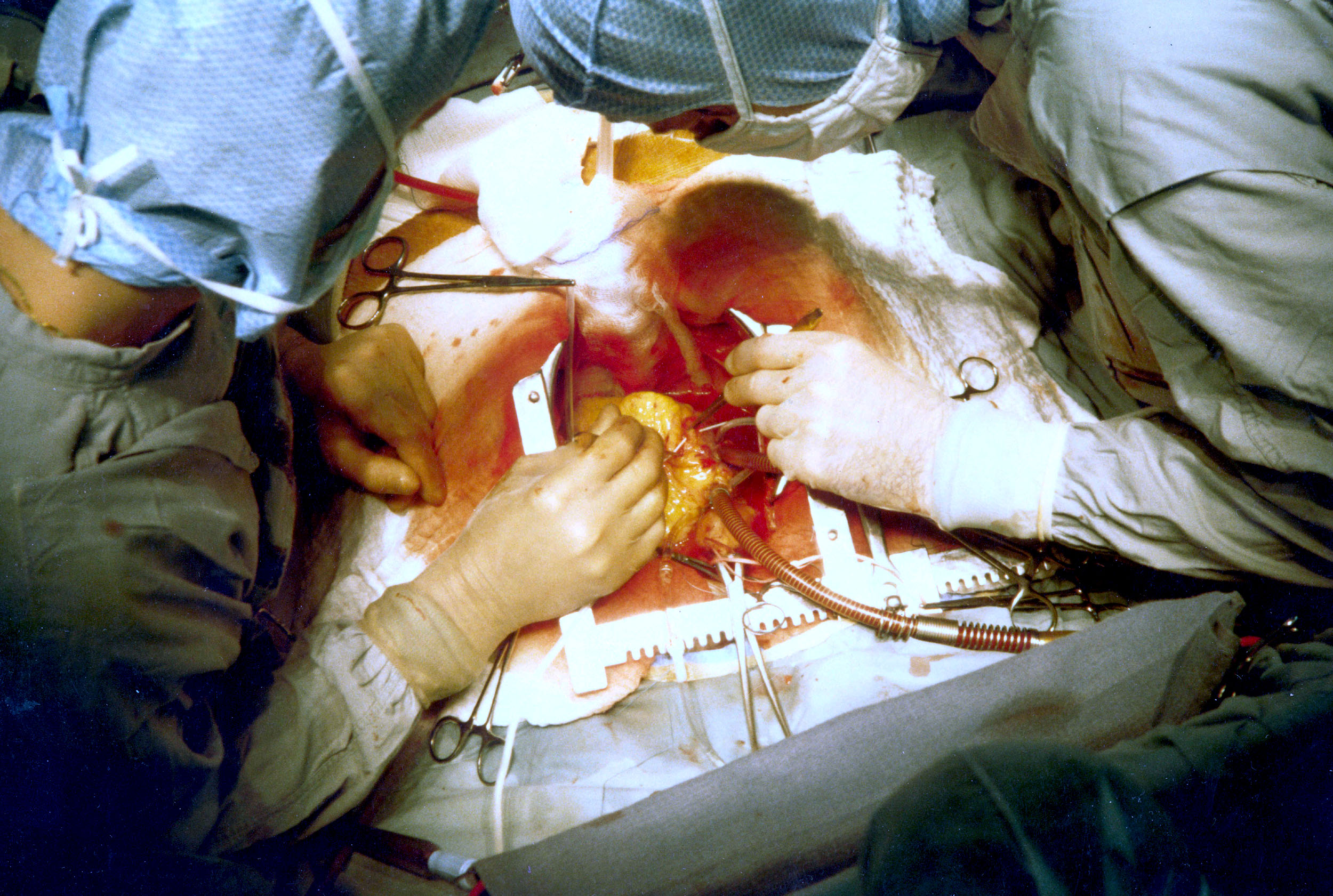
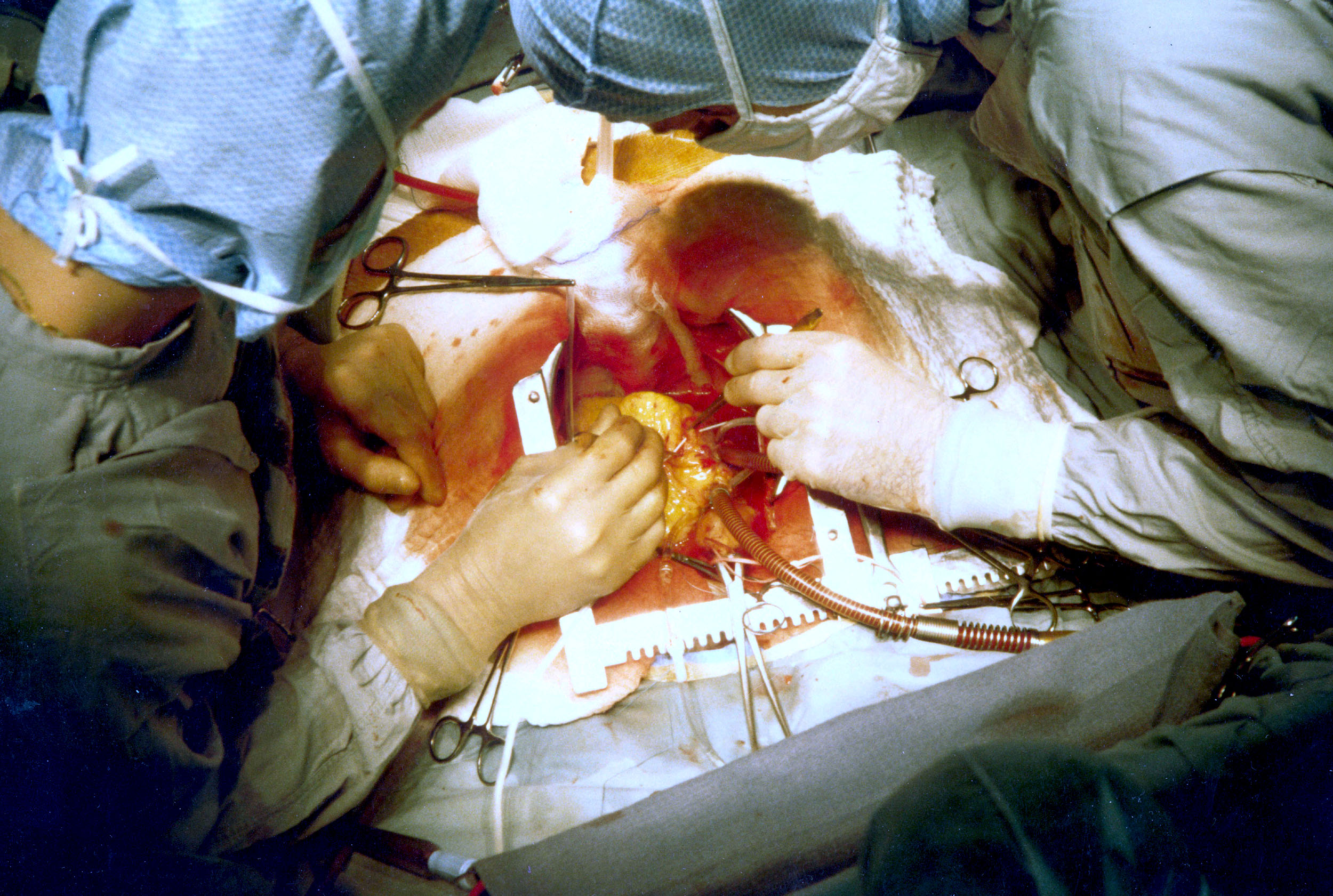
With CBP (on-pump)
The patient is brought to the operating theatre, intubated and lines (e.g., peripheral IV cannulae; central lines such as internal jugular cannulae) are inserted for drug administration and monitoring. The traditional way of a CABG follows: ; Harvesting A sternotomy is made, while conduits are being harvested (either from the arm or the leg). Then LITA (formerly, LIMA) is harvested through the sternotomy. There are two common ways of mobilizing the LITA, the pedicle (i.e., a pedicle consisting of the artery plus surrounding fat and veins) and the skeletonized (i.e., freed of other tissues). Before being divided in its more distal part, heparin is administered to the patient via a peripheral line (for clot prevention). ; Catheterization and establishment of cardiopulmonary bypass (on-pump) After harvesting, the pericardium is opened and stay sutures are placed to keep it open. Purse string sutures are placed in aorta to prepare the insertions of the aortic cannula and the catheter for cardioplegia (a solution high in potassium that serves to arrest the heart). Another purse string is placed in right atrium for the venous cannula. Then the cannulas and the catheter are placed, cardiopulmonary bypass is commenced (venous deoxygenated blood arriving to the heart is forwarded to the CBP machine to get oxygenated and delivered to aorta to keep rest of the body saturated, and often cooled to 32 - 34 degrees celsius in order to slow down the metabolism and minimize as much as possible the demand for oxygen. A clamp is placed on the Aorta between the cardioplegic catheter and aortic cannula, so the cardioplegic solution that the flow is controlled by the surgeon that clamps Aorta. Within minutes, heart stops beating. ; Anastomosis (grafting) With the heart still, the tip of the heart is taken out of pericardium, so the native arteries lying in the posterior side of the heart are accessible. Usually, distal anastomosis are constructed first (first to right coronary system, then to the circumflex) and then the sequential anastomosis if necessary. Surgeons check the anastomosis for patency or leaking and if everything is as it should be, surgeons insert the graft within the pericardium, sometimes attached to the cardioplegic catheter. The anastomosis of LIMA to LAD is usually the last one of the distal anastomoses to be constructed, while it is being constructed the rewarming process starts (by the CPB).. After the anastomosis is completed and checked for leaks, the proximal anastomoses of the conduits, if any, are next. They can be done either with the clamp still on or after removing the aortic clamp and isolating a small segment of the aorta by placing a partial clamp (but atheromatic aortas might be damaged by overhandling them; atheromatic derbis might get detached and cause embolization in end organs) ; Weaning from cardiopulmonary bypass and closure After the proximal anastomoses are done, the clamp is removed, aorta and conduits deaired, pacing wires might be placed if indicated and if the heart and other systems are functioning well CBP is discontinued, cannulas removed and protamine is administered to reverse the effect of heparin . After possible bleeding sites are checked, chest tubes are placed and sternum is closed.Off-pump (OPCABG)
Off-pump coronary artery bypass graft (OPCABG) surgery avoids using CPB machine by stabilizing small segments of the heart. It takes great care and coordination among the surgical team and anesthesiologists to not manipulate the heart too much so hemodynamic stability will not be compromised; however, if it is compromised, it should be detected immediately and appropriate action should be taken. To keep heart beating effectively, some maneuvers can take place like placing atrial wires to protect from bradycardia, placing stitches or incisions to pericardium to help exposure. Snares and tapes are used to facilitate exposure. the aim is to avoid distal ischemia by occluding the vessel supplying distal portions of the left ventricle, so usually LIMA to LAD is the first to be anastomosed and others follow. For the anastomosis, a fine tube blowing humidified CO2 is used to keep the surgical field clean of blood. Also, a shunt might be used so the blood can travel pass the anastomotic site. After the distal anastomosis are completed, proximal anastomosis to the aorta are constructed with a partially aortic clamp and rest is similar with on-pump CABG.Alternative approaches and special situations
When CABG is performed as an emergency because of hemodynamic compromise after an infraction, priority is to salvage the struggling myocardium. Pre-operatively, anintra-aortic balloon pump
The intra-aortic balloon pump (IABP) is a mechanical device that increases myocardial oxygen perfusion and indirectly increases cardiac output through afterload reduction. It consists of a cylindrical polyurethane balloon that sits in the aorta, ...
(IABP) might be inserted to relieve some of the burden of pumping blood, effectively reducing the amount of oxygen needed by myocardium. Operatively, the standard practice is to place the patient on CPB as soon as possible and revascularize the heart with three saphenous veins. Calcified aorta also poses a problem since it is very dangerous to clamp. In this case, the operation can be done as off-pump CAB utilizing both IMAs or Y, T and sequential grafts, or in deep hypothermic arrest, that is lower the temperature of the body to little above 20 Celsius, can also force the heart stop moving. In cases were a significant artery is totally occluded, there's a possibility to remove the atheroma, and using the same hole in the artery to perform an anastomosis ·this technique is called endarterectomy and is usually performed at the Right Coronary System.
Reoperations of CABG (another CABG operation after a previous one), poses some difficulties: Heart may be too close to the sternum and thus at risk when cutting the sternum again, so an oscillating saw is used. Heart may be covered with strong adhesions to adjusting structures, adding to the difficulty of the procedure. Also, aging grafts pose a dilemma, whether they should be replaced with new ones or not. Manipulation of vein grafts risks dislodgement of atheromatic debris and is avoided.
"Minimally Invasive revascularization" (commonly MIDCAB form minimally invasive direct coronary artery bypass) is a technique that strives to avoid a large sternotomy. It utilizes off pump techniques to place a graft, usually LIMA at LAD. LIMA is monilized through a left thoracotomy, or even endoscopically through a thoracoscope placed in the left chest. Robotic Coronary revascularization avoids the sternotomy to prevent infections and bleeding. Both conduit harvesting and the anastomosis are performed with the aid of a robot, through a thoracotomy. There is still no widespread use of the technique though. Usually it is combined with Hybrid Coronary Revascularization, which is the strategy where combined methods of CABG and PCI are employed. LIMA to LAD is performed in the operating theatre and other lesions are treated with PCI, either at the operating room, right after the anastomosis or serval days later.
After the procedure
After the procedure, the patient is usually transferred to the intensive care unit, where they are extubated if it hasn't been done already in the operating theatre. The following day they exit the ICU, and 4 days later, if no complications occur, the patient is discharged from the hospital. A series of drugs are commonly used in the early postoperative period. Dobutamine, a beta agent, can be used to increase the cardiac output that sometimes occurs some hours after the operation. Beta blockers are used to prevent atrial fibrillation and other supraventricular arrhythmias. Biatrial pacing through the pacing wires inserted at operation might help towards preventing atrial fibrillation. Aspirin 80mg is used to prevent graft failure.Angiotensin-converting enzyme (ACE) inhibitors
Angiotensin-converting-enzyme inhibitors (ACE inhibitors) are a class of medication used primarily for the treatment of hypertension, high blood pressure and heart failure. They work by causing relaxation of blood vessels as well as a decrease i ...
and Angiotensin receptor blockers (ARBs) are used to control blood pressure, especially in patients with low cardiac function (<40%). Amlodipine
Amlodipine, sold under the brand name Norvasc among others, is a calcium channel blocker medication used to treat high blood pressure and coronary artery disease. It is taken by mouth.
Common side effects include swelling, feeling tired, ab ...
, a calcium channel blocker, is used for patients that radial artery was used as a graft.
After the discharge, patients might suffer from insomnia, low appetite, decreased sex drive, and memory problems. This effect is usually transient and lasts 6 to 8 weeks. A tailored exercise plan usually benefits the patient.
Results
CABG is the best procedure to reduce mortality from severe CAD and improve quality of life. Operative mortality relates strongly to age of patient. According to a study by Eagle et al, for patients 50-59 years old there's an operative mortality rate of 1.8% while patients older than 80, the risk is 8.3%. Other factors which increase mortality are: female gender, re-operation, dysfunction of Left ventricle and left main disease. In most cases, CABG relieves angina, but in some patients it reoccurs in a later stage of their lives. Around 60% of patient will be angina free, 10 years after their operation. Myocardial infarction is rare 5 years after a CABG, but its prevalence increases with time. Also, the risk of sudden death is low for CABG patients. Quality of life is also high for at least 5 years, then starts to decline. The beneficial effects of CABG are clear at cardiac level. LV function is improved and malfunctioning segments of the heart (dyskinetic-moving inefficiently or even akinetic-not moving) can show signs of improvement. Both systolic and diastolic functions are improved and keep improving for up to 5 years in some cases. LV function, and myocardial perfusion, during exercise also improves after CABG. But when the LV function is severely impaired before operation (EF<30%), the benefits at the heart are less impressive in terms of segmental wall movement, but still significant since other parameters might improve as LV functions improves, the pulmonary hypertension might be relieved and survival is prolonged. It is hard to determine the total risk of the procedure since the group of patients undergoing CABG is a heterogeneous one, hence various subgroups have different risk, but it seems like the results for younger patients are better. Also, a CABG with two rather one internal mammary arteries seems to offer greater protection from CAD but results are not yet conclusive.Grafts
Various conduits can be utilized for CABG- they fall into two main categories, arteries and veins. Arteries have a superior long term patency, but veins are still largely in use due to practicality. Arterial grafts that can be used originate from the part of the Internal Mammary Artery (IMA) that runs near the edge of sternum and can easily be mobilized and anastomosed to the native target vessel of the heart. Left is most often used as it is closer to heart but Right IMA is utilized depending on patient and surgeon preferences. ITAs advantages are mostly due to their endothelial cells that produce factors (Endothelium-derived relaxing factor
Endothelium-derived relaxing factor (EDRF) is a name for a Chemical substance, substance that Robert F. Furchgott discovered had the eponymous properties. Today, it is firmly established this substance is nitric oxide (NO). Endothelium produces NO ...
and prostacyclin
Prostacyclin (also called prostaglandin I2 or PGI2) is a prostaglandin member of the eicosanoid family of lipid molecules. It inhibits platelet activation and is also an effective vasodilator.
When used as a drug, it is also known as epoprosteno ...
) that protect the artery from atherosclerosis and thus stenosis or occlusion. But using two ITAs has drawbacks, high rate of specific complications (deep sternal wound infections) in some subgroups of patients, mainly in obese and diabetic ones. Left radial artery and left Gastroepiploic artery can be used as well. Long term patency is influenced by the type of artery used, as well as intrinsic factors of the cardiac arterial circulation.
Venous grafts used are mostly great saphenous veins and in some cases lesser saphenous vein. Their patency rate is lower than arteries. Aspirin protects grafts from occlusion; adding clopidogrel does not improve rates.
CABG vs PCI
CABG and percutaneous coronary intervention (PCI) are the two modalities the medical community has to revascularize stenotic lesions of the cardiac arteries. Which one is preferable for each patient is still a matter of debate, but it is clear that in the presence of complex lesions, significant Left Main Disease and in diabetic patients, CABG seems to offer better results to patients than PCI. Strong indications for CABG also include symptomatic patients and in cases where LV function is impaired.History
Pre-CABG
Alexis Carrel
Alexis Carrel (; 28 June 1873 – 5 November 1944) was a French surgeon and biologist who was awarded the Nobel Prize in Physiology or Medicine in 1912 for pioneering vascular suturing techniques. He invented the first perfusion pump with Charle ...
was the first to anastomose a vessel (a branch of carotid artery) to a native artery in the Heart, in a canine model- but because of technical difficulties the operation could not be reproduced. In mid 20th century, revascularization efforts continued. Beck CS, used a carotid conduit to connect descending aorta to coronary sinus
In anatomy, the coronary sinus () is a collection of veins joined together to form a large vessel that collects blood from the heart muscle ( myocardium). It delivers deoxygenated blood to the right atrium, as do the superior and inferior ven ...
-the biggest vein of the heart, while Arthur Vineberg used skeletonized LIMA, placing it in a small tunnel he created next to LAD (known "Vineberg Procedure"), with the hope of spontaneous collateral circulation would form, and it did in canine experiments but was not successful in humans. Goetz RH was the first to perform an anastomosis of the IMA to LAD in the 1960 utilizing a sutureless technique.
The development of coronary angiography in 1962 by Mason Sones
F. Mason Sones, Jr. (October 28, 1918 – August 28, 1985) was an American physician whose pioneering work in cardiac catheterization was instrumental in the development of both coronary artery bypass surgery and interventional cardiology.
Earl ...
, helped medical doctors to identify both patients that are in need of operation, but also which native heart vessels should be bypassed. In 1964, Soviet cardiac surgeon, Vasilii Kolesov
Vasilii Ivanovich Kolesov (russian: Василий Иванович Колесов; 24 September 1904 – 2 August 1992) was one of the pioneers of global cardiac surgery. He was the first to perform successful internal coronary artery bypass sur ...
, performed the first successful internal mammary artery–coronary artery anastomosis, followed by Michael DeBakey
Michael Ellis DeBakey (September 7, 1908 – July 11, 2008) was a Lebanese-American general and cardiovascular surgeon, scientist and medical educator who became Chairman of the Department of Surgery, President, and Chancellor of Baylor College ...
in the USA. But it was René Favaloro
René Gerónimo Favaloro (July 12, 1923 – July 29, 2000) was an Argentine cardiac surgeon and educator best known for his pioneering work on coronary artery bypass surgery using the great saphenous vein.
Early life
Favaloro was born in 192 ...
that standarized the procedure. Their advances made CABG as the standard of care of CAD patients.
The CABG era
The "modern" era of the CABG begun in 1964 when the Soviet cardiac surgeonVasilii Kolesov
Vasilii Ivanovich Kolesov (russian: Василий Иванович Колесов; 24 September 1904 – 2 August 1992) was one of the pioneers of global cardiac surgery. He was the first to perform successful internal coronary artery bypass sur ...
performed the first successful internal mammary artery–coronary artery anastomosis in 1964, while Michael DeBakey
Michael Ellis DeBakey (September 7, 1908 – July 11, 2008) was a Lebanese-American general and cardiovascular surgeon, scientist and medical educator who became Chairman of the Department of Surgery, President, and Chancellor of Baylor College ...
used a saphenous vein to create an aorta-coronary artery bypass. The Argentinean surgeon Rene Favaloro advanced and standardized the CABG technique using the patient's saphenous vein.
Introduction of cardioplegia led to CABG becoming a much less risky operation. A major obstacle of CABG during those times were ischemia and infarction, occurring while the heart was stopped to allow surgeons to construct the distal anastomosis. In the 1970s potassium cardioplegia was utilized. Cardioplegia minimized the oxygen demands of the heart, thus the effects of ischemia were also minimized. Refinement of cardioplegia in the 1980s made CABG less risky (lowering perioperative mortality) and thus a more attractive option when dealing with CAD.
In the late 1960s, after the work of Rene Favaloro, the operation was still performed in a few centers of excellence, but was anticipated to change the landscape of Coronary Artery Disease, a significant killer in the developed world. More and more centers began performing CABG, resulting in 114,000 procedures/year in the USA by 1979. The introduction of PCI did not lead to the abandonment of CABG; the number of both procedures continued to increase, albeit PCIs grew more rapidly. In the following decades CABG was extensively studied and compared to PCI. The absence of a clear advantage of CABG over PCI led to a small decrease in numbers of CABGs in some countries (like the USA) at the turn of the millennium, but in European countries CABG was increasingly performed (mainly in Germany). Research is still ongoing on CABG vs PCI.
In the history of graft selection, again the work of Favaloro was fundamental. He established that the use of bilateral IMAs was superior to vein grafts. The following years, surgeons examined the use of other arterial grafts (splenic, gastroepiploic mesenteric, subscapular and others) but none of these matched the patency rates of IMA. Carpentier in 1971 introduced the us of the radial artery, which was initially prone to failure, but the evolution of harvesting techniques in the next two decades improved patency significantly.
See also
*Angioplasty
Angioplasty, is also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atheroscle ...
* Cardiothoracic surgery
Cardiothoracic surgery is the field of medicine involved in surgical treatment of organs inside the thoracic cavity — generally treatment of conditions of the heart ( heart disease), lungs (lung disease), and other pleural or mediastinal st ...
* Cleveland Clinic
Cleveland Clinic is a nonprofit American academic medical center based in Cleveland, Ohio. Owned and operated by the Cleveland Clinic Foundation, an Ohio nonprofit corporation established in 1921, it runs a 170-acre (69 ha) campus in Cleveland, ...
* Dressler's syndrome
Dressler syndrome is a secondary form of pericarditis that occurs in the setting of injury to the heart or the pericardium (the outer lining of the heart). It consists of fever, pleuritic pain, pericarditis and/or a pericardial effusion.
Dressle ...
* Hybrid coronary revascularization
Hybrid coronary revascularization (HCR) or hybrid coronary bypass is a relatively new type of heart surgery that provides an alternative to traditional coronary artery bypass surgery (CABG) or percutaneous coronary intervention (PCI or PTCA) by ...
* Totally endoscopic coronary artery bypass surgery
Totally Endoscopic Coronary Artery Bypass Surgery (TECAB) is an entirely endoscopic robotic surgery used to treat coronary heart disease, developed in the late 1990s. It is an advanced form of Minimally Invasive Coronary Artery Bypass Surgery, wh ...
* Chest tube
A chest tube (also chest drain, thoracic catheter, tube thoracostomy or intercostal drain) is a surgical drain that is inserted through the chest wall and into the pleural space or the mediastinum in order to remove clinically undesired substanc ...
References
Sources
* * * * * * * * * *External links
* Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, Bittl JA, Cohen MG, DiMaio JM, Don CW, Fremes SE, Gaudino MF, Goldberger ZD, Grant MC, Jaswal JB, Kurlansky PA, Mehran R, Metkus TS Jr, Nnacheta LC, Rao SV, Sellke FW, Sharma G, Yong CM, Zwischenberger BA. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:e21-e129 {{DEFAULTSORT:Coronary Artery Bypass Surgery Cardiac surgery