Antipsychotics, also known as neuroleptics,
are a class of
psychotropic medication
A psychoactive drug, psychopharmaceutical, psychoactive agent or psychotropic drug is a chemical substance, that changes functions of the nervous system, and results in alterations in perception, mood, consciousness, cognition or behavior.
Th ...
primarily used to manage
psychosis
Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior ...
(including
delusion
A delusion is a false fixed belief that is not amenable to change in light of conflicting evidence. As a pathology, it is distinct from a belief based on false or incomplete information, confabulation, dogma, illusion, hallucination, or some o ...
s,
hallucinations,
paranoia
Paranoia is an instinct or thought process that is believed to be heavily influenced by anxiety or fear, often to the point of delusion and irrationality. Paranoid thinking typically includes persecutory beliefs, or beliefs of conspiracy concer ...
or
disordered thought
A thought disorder (TD) is any disturbance in cognition that adversely affects language and thought content, and thereby communication. A variety of thought disorders were said to be characteristic of people with schizophrenia. A content-though ...
), principally in
schizophrenia
Schizophrenia is a mental disorder characterized by continuous or relapsing episodes of psychosis. Major symptoms include hallucinations (typically hearing voices), delusions, and disorganized thinking. Other symptoms include social withdra ...
but also in a range of other psychotic disorders.
They are also the mainstay together with
mood stabilizer
A mood stabilizer is a psychiatric medication used to treat mood disorders characterized by intense and sustained mood shifts, such as bipolar disorder and the bipolar type of schizoaffective disorder.
Uses
Mood stabilizers are best known for th ...
s in the treatment of
bipolar disorder
Bipolar disorder, previously known as manic depression, is a mental disorder characterized by periods of depression and periods of abnormally elevated mood that last from days to weeks each. If the elevated mood is severe or associated with ...
.
Prior research has shown that use of any antipsychotic is associated with smaller brain tissue volumes,
[ including ]white matter
White matter refers to areas of the central nervous system (CNS) that are mainly made up of myelinated axons, also called tracts. Long thought to be passive tissue, white matter affects learning and brain functions, modulating the distribution ...
reduction[ and that this brain shrinkage is dose dependent and time dependent.]pallidal
The globus pallidus (GP), also known as paleostriatum or dorsal pallidum, is a subcortical structure of the brain. It consists of two adjacent segments, one external, known in rodents simply as the globus pallidus, and one internal, known in rod ...
brain volume loss in first episode psychosis.metabolic syndrome
Metabolic syndrome is a clustering of at least three of the following five medical conditions: abdominal obesity, high blood pressure, high blood sugar, high serum triglycerides, and low serum high-density lipoprotein (HDL).
Metabolic syndrome ...
. Long-term use can produce adverse effects such as tardive dyskinesia, tardive dystonia, and tardive akathisia.
Prevention of these adverse effects is possible through concomitant medication strategies including use of beta-blockers. Currently, treatments for tardive diseases are not well established.
First-generation antipsychotics (e.g. chlorpromazine), known as typical antipsychotics, were first introduced in the 1950s, and others were developed until the early 1970s.
Medical uses
Antipsychotics are most frequently used for the following conditions:
* Schizophreniaantidepressant
Antidepressants are a class of medication used to treat major depressive disorder, anxiety disorders, chronic pain conditions, and to help manage addictions. Common side-effects of antidepressants include dry mouth, weight gain, dizziness, hea ...
(in the case of the depressive subtype) or a mood stabiliser (in the case of the bipolar subtype).
* Bipolar disorder (acute mania and mixed episodes) may be treated with either typical or atypical antipsychotics, although atypical antipsychotics are usually preferred because they tend to have more favourable adverse effect profiles[ and, according to a recent meta-analysis, they tend to have a lower liability for causing conversion from mania to depression.][
* Treatment resistant depression as an adjunct to standard antidepressant therapy.][ There are evidence-based indications for using antipsychotics in children (e.g. tic disorder, bipolar disorder, psychosis), but the use of antipsychotics outside of those contexts (e.g. to treat behavioral problems) warrants significant caution.][
Antipsychotics are used to treat tics associated with Tourette syndrome. Aripiprazole, an atypical antipsychotic, is used as add-on medication to ameliorate sexual dysfunction as a symptom of Selective serotonin reuptake inhibitor antidepressants in women. Quetiapine is used to treat generalized anxiety disorder.
]
Schizophrenia
Antipsychotic drug treatment is a key component of schizophrenia treatment recommendations by the National Institute of Health and Care Excellence (NICE),positive symptoms
Signs and symptoms are the observed or detectable signs, and experienced symptoms of an illness, injury, or condition. A sign for example may be a higher or lower temperature than normal, raised or lowered blood pressure or an abnormality showin ...
of psychosis that include delusions and hallucinations.
Prevention of psychosis and symptom improvement
Test batteries such as the PACE (Personal Assessment and Crisis Evaluation Clinic) and COPS (Criteria of Prodromal Syndromes), which measure low-level psychotic symptoms and cognitive disturbances, are used to evaluate people with early, low-level symptoms of psychosis. Test results are combined with family history information to identify patients in the "high-risk" group; they are considered to have a 20ā40% risk of progression to frank psychosis within two years.[ These patients are often treated with low doses of antipsychotic drugs with the goal of reducing their symptoms and preventing progression to frank psychosis. While generally useful for reducing symptoms, clinical trials to date show little evidence that early use of antipsychotics improves long-term outcomes in those with prodromal symptoms, either alone or in combination with cognitive-behavioral therapy.
]
First episode psychosis
First episode psychosis (FEP) is the first time that psychotic symptoms are presented. NICE recommends that all persons presenting with first episode psychosis be treated with both an antipsychotic drug, and cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. CBT focuses on challenging and changing cognitive distortions (suc ...
(CBT). NICE further recommends that those expressing a preference for CBT alone are informed that combination treatment is more effective.drug induced psychosis
Stimulant psychosis is a mental disorder characterized by psychotic symptoms (such as hallucinations, paranoid ideation, delusions, Thought disorder, disorganized thinking, grossly disorganized behaviour) which involves and typically occurs follow ...
to bipolar disorder or schizophrenia are lower, with 30% of people converting to either bipolar disorder or schizophrenia.
Recurrent psychotic episodes
Placebo-controlled trials of both first and second generation antipsychotic drugs consistently demonstrate the superiority of active drug to placebo in suppressing psychotic symptoms.
Maintenance therapy
The majority of patients treated with an antipsychotic drug will experience a response within four weeks. The goals of continuing treatment are to maintain suppression of symptoms, prevent relapse, improve quality of life, and support engagement in psychosocial therapy.involuntary commitment
Involuntary commitment, civil commitment, or involuntary hospitalization/hospitalisation is a legal process through which an individual who is deemed by a qualified agent to have symptoms of severe mental disorder is detained in a psychiatric hos ...
, in which they can be forced to accept treatment (including antipsychotics). A person can also be committed to treatment outside of a hospital, called outpatient commitment.
Antipsychotics in long-acting injectable (LAI), or "depot", form have been suggested as a method of decreasing medication nonadherence (sometimes also called non-compliance).
Bipolar disorder
Antipsychotics are routinely used, often in conjunction with mood stabilisers such as lithium/ valproate, as a first-line treatment for manic and mixed episodes associated with bipolar disorder.[
At least five atypical antipsychotics (]lumateperone
Lumateperone, sold under the brand name Caplyta, is an atypical antipsychotic medication of the butyrophenone class. It is approved for the treatment of schizophrenia as well as bipolar depression, as either monotherapy or adjunctive therapy (wi ...
, cariprazine, lurasidone
Dementia
Psychosis and agitation develop in as many as 80 percent of people living in nursing homes.
Major depressive disorder
A number of atypical antipsychotics have some benefits when used in addition to other treatments in major depressive disorder.fluoxetine
Fluoxetine, sold under the brand names Prozac and Sarafem, among others, is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. It is used for the treatment of major depressive disorder, obsessiveācompulsive disorde ...
) have received the Food and Drug Administration (FDA) labelling for this indication.[Truven Health Analytics, Inc. DrugPoint System (Internet) ited 2013 Oct 2 Greenwood Village, CO: Thomsen Healthcare; 2013.] There is, however, a greater risk of side effects with their use compared to using traditional antidepressants.
Other
Besides the above uses antipsychotics may be used for obsessiveācompulsive disorder, post-traumatic stress disorder, personality disorders, Tourette syndrome, autism
The autism spectrum, often referred to as just autism or in the context of a professional diagnosis autism spectrum disorder (ASD) or autism spectrum condition (ASC), is a neurodevelopmental condition (or conditions) characterized by difficulti ...
and agitation in those with dementia.[ Evidence however does not support the use of atypical antipsychotics in ]eating disorder
An eating disorder is a mental disorder defined by abnormal eating behaviors that negatively affect a person's physical or mental health. Only one eating disorder can be diagnosed at a given time. Types of eating disorders include binge eating d ...
s or personality disorder.neutropenia
Neutropenia is an abnormally low concentration of neutrophils (a type of white blood cell) in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteria ...
, and a recent network meta-analysis of 154 double-blind, randomized controlled trials of drug therapies vs. placebo for insomnia in adults found that quetiapine did not demonstrated any short-term benefits in sleep quality. Low dose antipsychotics may also be used in treatment of impulse-behavioural and cognitive-perceptual symptoms of borderline personality disorder
Borderline personality disorder (BPD), also known as emotionally unstable personality disorder (EUPD), is a personality disorder characterized by a long-term pattern of unstable interpersonal relationships, distorted sense of self, and strong ...
.
In children they may be used in those with disruptive behavior disorder
DSM-IV codes are the classification found in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision, also known as ''DSM-IV-TR'', a manual published by the American Psychiatric Association (APA) that includes almost a ...
s, mood disorders and pervasive developmental disorder
The diagnostic category pervasive developmental disorders (PDD), as opposed to specific developmental disorders (SDD), is a group of disorders characterized by delays in the development of multiple basic functions including socialization and co ...
s or intellectual disability. Antipsychotics are only weakly recommended for Tourette syndrome, because although they are effective, side effects are common. The situation is similar for those on the autism spectrum.
Much of the evidence for the off-label use of antipsychotics (for example, for dementia, OCD, PTSD, Personality Disorders, Tourette's) was of insufficient scientific quality to support such use, especially as there was strong evidence of increased risks of stroke, tremors, significant weight gain, sedation, and gastrointestinal problems. A UK review of unlicensed usage in children and adolescents reported a similar mixture of findings and concerns. A survey of children with pervasive developmental disorder
The diagnostic category pervasive developmental disorders (PDD), as opposed to specific developmental disorders (SDD), is a group of disorders characterized by delays in the development of multiple basic functions including socialization and co ...
found that 16.5% were taking an antipsychotic drug, most commonly for irritability, aggression, and agitation. Both risperidone and aripiprazole have been approved by the US FDA for the treatment of irritability in autistic children and adolescents.[Truven Health Analytics, Inc. DRUGDEX System (Internet) ited 2013 Oct 10 Greenwood Village, CO: Thomsen Healthcare; 2013.]
Aggressive challenging behavior in adults with intellectual disability is often treated with antipsychotic drugs despite lack of an evidence base. A recent randomized controlled trial, however, found no benefit over placebo and recommended that the use of antipsychotics in this way should no longer be regarded as an acceptable routine treatment.
Antipsychotics may be an option, together with stimulants, in people with ADHD and aggressive behavior when other treatments have not worked. They have not been found to be useful for the prevention of delirium
Delirium (also known as acute confusional state) is an organically caused decline from a previous baseline of mental function that develops over a short period of time, typically hours to days. Delirium is a syndrome encompassing disturbances in ...
among those admitted to hospital.
Typicals vs atypicals
It is unclear whether the atypical (second-generation) antipsychotics offer advantages over older, first generation antipsychotics.agranulocytosis
Agranulocytosis, also known as agranulosis or granulopenia, is an acute condition involving a severe and dangerous lowered white blood cell count (leukopenia, most commonly of neutrophils) and thus causing a neutropenia in the circulating blood. ...
(lowered white blood cell
White blood cells, also called leukocytes or leucocytes, are the cell (biology), cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and de ...
count) in less than 4% of people.
Due to bias in the research the accuracy of comparisons of atypical antipsychotics is a concern.
In 2005, a US government body, the National Institute of Mental Health published the results of a major independent study (the CATIE project). No other atypical studied ( risperidone, quetiapine, and ziprasidone) did better than the typical perphenazine on the measures used, nor did they produce fewer adverse effects than the typical antipsychotic perphenazine, although more patients discontinued perphenazine owing to extrapyramidal effects
Extrapyramidal symptoms (EPS) are symptoms that are archetypically associated with the extrapyramidal system of the brain's cerebral cortex. When such symptoms are caused by medications or other drugs, they are also known as extrapyramidal side ...
compared to the atypical agents (8% vs. 2% to 4%).
Adverse effects
Generally, more than one antipsychotic drug should not be used at a time because of increased adverse effects.[, which cites
*
*
* ]
Some atypicals are associated with considerable weight gain, diabetes and the risk of metabolic syndrome
Metabolic syndrome is a clustering of at least three of the following five medical conditions: abdominal obesity, high blood pressure, high blood sugar, high serum triglycerides, and low serum high-density lipoprotein (HDL).
Metabolic syndrome ...
.tardive psychosis Tardive psychosis is a term for a hypothetical form of psychosis, proposed in 1978. It was defined as a condition caused by long term use of neuroleptics, noticeable when the medication had become decreasingly effective, requiring higher doses, or w ...
.
Clozapine is associated with side effects that include weight gain, tiredness, and hypersalivation. More serious adverse effects include seizures, NMS, neutropenia
Neutropenia is an abnormally low concentration of neutrophils (a type of white blood cell) in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteria ...
, and agranulocytosis
Agranulocytosis, also known as agranulosis or granulopenia, is an acute condition involving a severe and dangerous lowered white blood cell count (leukopenia, most commonly of neutrophils) and thus causing a neutropenia in the circulating blood. ...
(lowered white blood cell
White blood cells, also called leukocytes or leucocytes, are the cell (biology), cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and de ...
count) and its use needs careful monitoring.myocarditis
Myocarditis, also known as inflammatory cardiomyopathy, is an acquired cardiomyopathy due to inflammation of the heart muscle. Symptoms can include shortness of breath, chest pain, decreased ability to exercise, and an irregular heartbeat. The ...
, and cardiomyopathy
Cardiomyopathy is a group of diseases that affect the heart muscle. Early on there may be few or no symptoms. As the disease worsens, shortness of breath, feeling tired, and swelling of the legs may occur, due to the onset of heart failure. A ...
.bowel ischemia
Intestinal ischemia is a medical condition in which injury to the large or small intestine occurs due to not enough blood supply. It can come on suddenly, known as acute intestinal ischemia, or gradually, known as chronic intestinal ischemia. The ...
resulting in many fatalities.
By rate
Common (ā„ 1% and up to 50% incidence for ''most'' antipsychotic drugs) adverse effects of antipsychotics include:
* Sedation (particularly common with asenapine, clozapine, olanzapine, quetiapine, chlorpromazine and zotepineExtrapyramidal side effects
Extrapyramidal symptoms (EPS) are symptoms that are archetypically associated with the extrapyramidal system of the brain's cerebral cortex. When such symptoms are caused by medications or other drugs, they are also known as extrapyramidal side ...
(particularly common with first-generation antipsychotics), which include:
:- Akathisia, an often distressing sense of inner restlessness.
:- Dystonia
Dystonia is a neurological hyperkinetic movement disorder in which sustained or repetitive muscle contractions result in twisting and repetitive movements or abnormal fixed postures. The movements may resemble a tremor. Dystonia is often inten ...
, an abnormal muscle contraction
:- Pseudoparkinsonism
Parkinsonism is a clinical syndrome characterized by tremor, bradykinesia (slowed movements), Rigidity (neurology), rigidity, and balance disorder, postural instability. These are the four Parkinson's disease#Motor, motor symptoms found in Parkins ...
, symptoms that are similar to what people with Parkinson's disease experience, including tremulousness and drooling
* Hyperprolactinaemia (rare for those treated with clozapine, quetiapine and aripiprazoleGalactorrhoea
Galactorrhea ( also spelled galactorrhoea) ( galacto- + -rrhea) or lactorrhea ( lacto- + -rrhea) is the spontaneous flow of milk from the breast, unassociated with childbirth or nursing.
Galactorrhea is reported to occur in 5ā32% of women. M ...
, the unusual secretion of breast milk.
:- Gynaecomastia, abnormal growth of breast tissue
:- Sexual dysfunction (in both sexes)
:- Osteoporosis
* Orthostatic hypotension
* Weight gain (particularly prominent with clozapine, olanzapine, quetiapine and zotepineMetabolic syndrome
Metabolic syndrome is a clustering of at least three of the following five medical conditions: abdominal obesity, high blood pressure, high blood sugar, high serum triglycerides, and low serum high-density lipoprotein (HDL).
Metabolic syndrome ...
and other metabolic problems such as type II diabetes mellitus ā particularly common with clozapine, olanzapine and zotepine. In American studies African Americans
African Americans (also referred to as Black Americans and Afro-Americans) are an ethnic group consisting of Americans with partial or total ancestry from sub-Saharan Africa. The term "African American" generally denotes descendants of ens ...
appeared to be at a heightened risk for developing type II diabetes mellitus. Evidence suggests that females are more sensitive to the metabolic side effects of first-generation antipsychotic drugs than males. Metabolic adverse effects appear to be mediated by the following mechanisms:
:- Causing weight gain by antagonizing the histamine H1 and serotonin 5-HT2CreceptorsQT interval
The QT interval is a measurement made on an electrocardiogram used to assess some of the electrical properties of the heart. It is calculated as the time from the start of the Q wave to the end of the T wave, and approximates to the time taken ...
prolongation ā more prominent in those treated with amisulpride, pimozide, sertindole, thioridazine and ziprasidone.Stroke
A stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functionin ...
Long-term effects
Some studies have found decreased life expectancy associated with the use of antipsychotics, and argued that more studies are needed. Antipsychotics may also increase the risk of early death in individuals with dementia. Antipsychotics typically worsen symptoms in people with depersonalisation disorder.
Discontinuation
The '' British National Formulary'' recommends a gradual withdrawal when discontinuing antipsychotics to avoid acute withdrawal syndrome or rapid relapse.[ Less commonly there may be a feeling of the world spinning, numbness, or muscle pains.][ Symptoms generally resolve after a short period of time.][
There is tentative evidence that discontinuation of antipsychotics can result in psychosis.][
Unexpected psychotic episodes have been observed in patients withdrawing from clozapine. This is referred to as ]supersensitivity psychosis
Dopamine supersensitivity psychosis is a hypothesis that attempts to explain the phenomenon in which psychosis (e.g. having hallucinations, which can mean hearing or seeing things that other people do not see or hear) occurs despite treatment with ...
, not to be equated with tardive dyskinesia.
List of agents


 Clinically used antipsychotic medications are listed below by drug group. Trade names appear in parentheses. A 2013 review has stated that the division of antipsychotics into first and second generation is perhaps not accurate.
Clinically used antipsychotic medications are listed below by drug group. Trade names appear in parentheses. A 2013 review has stated that the division of antipsychotics into first and second generation is perhaps not accurate.
First-generation (typical)
Butyrophenones
* Benperidol
Benperidol, sold under the trade name Anquil among others, is a typical antipsychotic primarily used to treat hypersexuality syndromes and can be used to treat schizophrenia. It is a highly potent butyrophenone derivative and is the most potent n ...
ā”
* Bromperidolā
* Droperidol
Droperidol (Inapsine, Droleptan, Dridol, Xomolix, Innovar ombination with fentanyl">fentanyl.html" ;"title="ombination with fentanyl">ombination with fentanyl is an antidopaminergic medication, drug used as an antiemetic (that is, to prevent o ...
ā”
* Haloperidol
* Moperone (''discontinued'')ā
* Pipamperone (''discontinued'')ā
* Timiperone
Timiperone, sold under the brand name Tolopelon, is a typical antipsychotic of the butyrophenone class which is marketed in Japan for the treatment of schizophrenia. It is similar in chemical structure to benperidol, but has a thiourea group ins ...
ā
Diphenylbutylpiperidines
* Fluspirilene ā”
* Penfluridol ā”
* Pimozide
Phenothiazines
* Acepromazine ā ā although it is mostly used in veterinary medicine.
* Chlorpromazine
* Cyamemazine ā
* Dixyrazine
Dixyrazine, also known as dixypazin (oxalate), sold under the brand names Ansiolene, Esocalm, Esucos, Metronal, and Roscal, is a typical antipsychotic of the phenothiazine group described as a neuroleptic and antihistamine. It was first introduced ...
ā
* Fluphenazine
* Levomepromazineā”
* Mesoridazine (''discontinued'')ā
* Perazine
Perazine (Taxilan) is a moderate-potency typical antipsychotic of the phenothiazine class. It is quite similar to chlorpromazine, and acts as a dopamine antagonist. A 2014 systematic review compared it with other antipsychotic drugs:
Synthe ...
* Pericyazine
Periciazine (INN), also known as pericyazine ( BAN) or propericiazine, is a drug that belongs to the phenothiazine class of typical antipsychotics.
Periciazine is not approved for sale in the United States. It is commonly sold in Canada, Italy ...
ā”
* Perphenazine
* Pipotiazine ā”
* Prochlorperazine
* Promazine (''discontinued'')
* Promethazine
* Prothipendyl ā
* Thioproperazineā” (only English-speaking country it is available in is Canada)
* Thioridazine (''discontinued'')
* Trifluoperazine
Trifluoperazine, marketed under the brand name Stelazine among others, is a typical antipsychotic primarily used to treat schizophrenia. It may also be used short term in those with generalized anxiety disorder but is less preferred to benzodiaze ...
* Triflupromazine
Triflupromazine (Vesprin) is an antipsychotic medication of the phenothiazine class. Among different effects of triflupromazine indication for use of this drug is severe emesis and severe Hiccups. Due to its potential side effects (triflupromazine ...
(''discontinued'')ā
Thioxanthenes
* Chlorprothixene ā
* Clopenthixol
* Flupentixol ā”
* Thiothixene
* Zuclopenthixol ā”
Disputed/unknown
This category is for drugs that have been called both first and second-generation, depending on the literature being used.
Benzamides
* Sulpiride ā”
* Sultopride
Sultopride (trade names Barnetil, Barnotil, Topral) is an atypical antipsychotic of the benzamide chemical class used in Europe, Japan, and Hong Kong for the treatment of schizophrenia. It was launched by Sanofi-Aventis in 1976. Sultopride acts a ...
ā
* Veralipride
Veralipride (Agreal, Agradil) is a typical antipsychotic of the benzamide class. It is indicated for the treatment of vasomotor symptoms associated with menopause. It is a D2 receptor antagonist and it induces prolactin secretion without any estr ...
ā
Tricyclics
* Carpipramine ā
* Clocapramine ā
* Clorotepine
Clorotepine (; brand names Clotepin, Clopiben), also known as octoclothepin or octoclothepine, is an antipsychotic of the tricyclic group which was derived from perathiepin in 1965 and marketed in the Czech Republic by Spofa in or around 1971 fo ...
ā
* Clotiapine
Clotiapine (Entumine) is an atypical antipsychotic of the dibenzothiazepine chemical class. It was first introduced in a few European countries (namely, Belgium, Italy, Spain and Switzerland), Argentina, Taiwan and Israel in 1970.
Some sources r ...
ā”
* Loxapine
* Mosapramine ā
Others
* Molindone #
Second-generation (atypical)
Benzamides
* Amisulpride ā” ā Selective dopamine antagonist. Higher doses (greater than 400 mg) act upon post-synaptic dopamine receptors resulting in a reduction in the positive symptoms of schizophrenia, such as psychosis. Lower doses, however, act upon dopamine autoreceptors, resulting in increased dopamine transmission, improving the negative symptoms of schizophrenia. Lower doses of amisulpride have also been shown to have antidepressant
Antidepressants are a class of medication used to treat major depressive disorder, anxiety disorders, chronic pain conditions, and to help manage addictions. Common side-effects of antidepressants include dry mouth, weight gain, dizziness, hea ...
and anxiolytic effects in non-schizophrenic patients, leading to its use in dysthymia and social phobias
Social anxiety disorder (SAD), also known as social phobia, is an anxiety disorder characterized by sentiments of fear and anxiety in social situations, causing considerable distress and impaired ability to function in at least some aspects ...
.
* Nemonapride
Nemonapride (ćØćć¬ć¼ć¹, Emilace ( JP)) is an atypical antipsychotic approved in Japan for the treatment of schizophrenia. It was launched by Yamanouchi in May 1991. Nemonapride acts as a D2 and D3 receptor antagonist, and is also a p ...
ā ā Used in Japan.
* Remoxipride
Remoxipride (Roxiam) is an atypical antipsychotic (although according to some sources it is a typical antipsychotic) which was previously used in Europe for the treatment of schizophrenia and acute mania but was withdrawn due to toxicity concern ...
# ā Has a risk of causing aplastic anaemia and, hence, has been withdrawn from the market worldwide. It has also been found to possess relatively low (virtually absent) potential to induce hyperprolactinaemia and extrapyramidal symptoms, likely attributable to its comparatively weak binding to (and, hence, rapid dissociation from) the D2 receptor.Sultopride
Sultopride (trade names Barnetil, Barnotil, Topral) is an atypical antipsychotic of the benzamide chemical class used in Europe, Japan, and Hong Kong for the treatment of schizophrenia. It was launched by Sanofi-Aventis in 1976. Sultopride acts a ...
ā An atypical antipsychotic of the benzamide chemical class used in Europe, Japan, and Hong Kong for the treatment of schizophrenia. It was launched by Sanofi-Aventis in 1976. Sultopride acts as a selective D2 and D3 receptor antagonist.
Benzisoxazoles/benzisothiazoles
* Lumateperone
Lumateperone, sold under the brand name Caplyta, is an atypical antipsychotic medication of the butyrophenone class. It is approved for the treatment of schizophrenia as well as bipolar depression, as either monotherapy or adjunctive therapy (wi ...
ā In December 2019, lumateperone received its first global approval in the USA for the treatment of schizophrenia in adults. In 2020 and 2021 FDA approved for depressive episodes associated with bipolar I or II disorder (bipolar depression) in adults, as monotherapy and as adjunctive therapy with lithium or valproate.
* Iloperidone ā Approved by the US FDA in 2009, it is fairly well tolerated, although hypotension, dizziness, and somnolence were very common side effects. Has not received regulatory approval in other countries, however.
* Paliperidone ā Primary, active metabolite of risperidone that was approved in 2006.
* Perospirone ā ā Has a higher incidence of extrapyramidal side effects than other atypical antipsychotics.anxiety disorder
Anxiety disorders are a cluster of mental disorders characterized by significant and uncontrollable feelings of anxiety and fear such that a person's social, occupational, and personal function are significantly impaired. Anxiety may cause physi ...
.
* Ziprasidone ā Approved in 2004 to treat bipolar disorder. Side-effects include a prolonged QT interval
The QT interval is a measurement made on an electrocardiogram used to assess some of the electrical properties of the heart. It is calculated as the time from the start of the Q wave to the end of the T wave, and approximates to the time taken ...
in the heart, which can be dangerous for patients with heart disease
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels. CVD includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack). Other CVDs include stroke, hea ...
or those taking other drugs that prolong the QT interval.
Butyrophenones
* Melperone ā ā Only used in a few European countries. No English-speaking country has licensed it to date.
* Lumateperone
Lumateperone, sold under the brand name Caplyta, is an atypical antipsychotic medication of the butyrophenone class. It is approved for the treatment of schizophrenia as well as bipolar depression, as either monotherapy or adjunctive therapy (wi ...
Tricyclics
* Asenapine ā Used for the treatment of schizophrenia and acute mania associated with bipolar disorder.
* Clozapine ā Requires routine laboratory monitoring of complete blood counts every one to four weeks due to the risk of agranulocytosis
Agranulocytosis, also known as agranulosis or granulopenia, is an acute condition involving a severe and dangerous lowered white blood cell count (leukopenia, most commonly of neutrophils) and thus causing a neutropenia in the circulating blood. ...
. It has unparalleled efficacy in the treatment of treatment-resistant schizophrenia.
* Olanzapine ā Used to treat psychotic disorders including schizophrenia, acute manic episodes, and maintenance of bipolar disorder
Bipolar disorder, previously known as manic depression, is a mental disorder characterized by periods of depression and periods of abnormally elevated mood that last from days to weeks each. If the elevated mood is severe or associated with ...
. Used as an adjunct to antidepressant therapy, either alone or in combination with fluoxetine
Fluoxetine, sold under the brand names Prozac and Sarafem, among others, is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. It is used for the treatment of major depressive disorder, obsessiveācompulsive disorde ...
as Symbyax.
* Quetiapine ā Used primarily to treat bipolar disorder and schizophrenia. Also used and licensed in a few countries (including Australia, the United Kingdom and the United States) as an adjunct to antidepressant therapy in patients with major depressive disorder. It's the only antipsychotic that's demonstrated efficacy as a monotherapy for the treatment of major depressive disorder. It indirectly serves as a norepinephrine reuptake inhibitor by means of its active metabolite, norquetiapine.
* Zotepine ā An atypical antipsychotic indicated for acute and chronic schizophrenia. It is still used in Japan and was once used in Germany but it was discontinued.ā
Others
* Blonanserin ā Approved by the PMDA in 2008. Used in Japan and South Korea.
* Pimavanserin ā A selective 5-HT2A receptor antagonist approved for the treatment of Parkinson's disease psychosis in 2016.
* Sertindole ā” ā Developed by the Danish pharmaceutical company H. Lundbeck
H. Lundbeck A/S (commonly known simply as Lundbeck) is a Danish international pharmaceutical company engaged in the research, development, manufacturing, marketing and sale of pharmaceuticals across the world. The companyās products are target ...
. Like the other atypical antipsychotics, it is believed to have antagonist
An antagonist is a character in a story who is presented as the chief foe of the protagonist.
Etymology
The English word antagonist comes from the Greek į¼Ī½ĻĪ±Ī³ĻĪ½Ī¹ĻĻĪ®Ļ ā ''antagonistÄs'', "opponent, competitor, villain, enemy, riv ...
activity at dopamine and serotonin receptors in the brain.
Third-generation
Third generation antipsychotics are recognized as demonstrating D2 receptor agonism
Agonism (from Greek į¼Ī³ĻĪ½ '' agon'', "struggle") is a political and social theory that emphasizes the potentially positive aspects of certain forms of conflict. It accepts a permanent place for such conflict in the political sphere, but seeks ...
as opposed to the D2 receptor antagonistic mechanism of both first-generation (typical) and second-generation (atypical) antipsychotic medications.
Phenylpiperazines/quinolinones
* Aripiprazole (Abilify) ā Partial agonist at the D2 receptor. Considered the prototypical third-generation antipsychotic.
* Aripiprazole lauroxil
Aripiprazole lauroxil, sold under the brand name Aristada, is a long-acting injectable atypical antipsychotic that was developed by Alkermes. It is an N-acyloxymethyl prodrug of aripiprazole that is administered via intramuscular injection once ...
(Abilify Maintena)ā Long-acting version of aripiprazole for injection.
* Brexpiprazole
Brexpiprazole, sold under the brand name Rexulti among others, is an atypical antipsychotic. It is a dopamine D2 receptor partial agonist and has been described as a "serotoninādopamine activity modulator" (SDAM). The drug was approved by t ...
ā Partial agonist of the D2 receptor. Successor of aripiprazole.
* Cariprazine ā A D3-preferring D2/D3 partial agonist.
= Benzisoxazoles/benzisothiazoles
=
* Lurasidone (Latuda) ā Approved by the US FDA for schizophrenia and bipolar depression, and for use as schizophrenia treatment in Canada.
Mechanism of action
Antipsychotic drugs such as haloperidol and chlorpromazine tend to block dopamine
Dopamine (DA, a contraction of 3,4-dihydroxyphenethylamine) is a neuromodulatory molecule that plays several important roles in cells. It is an organic compound, organic chemical of the catecholamine and phenethylamine families. Dopamine const ...
D2 receptors in the dopaminergic pathways of the brain. This means that dopamine released in these pathways has less effect. Excess release of dopamine in the mesolimbic pathway has been linked to psychotic experiences. Decreased dopamine release in the prefrontal cortex, and excess dopamine release in other pathways, are associated with psychotic episodes in schizophrenia and bipolar disorder.
In addition to the antagonistic effects of dopamine, antipsychotics (in particular atypical neuroleptics) also antagonize 5-HT2A receptors. Different alleles of the 5-HT2A receptor have been associated with schizophrenia and other psychoses, including depression.
Comparison of medications
History
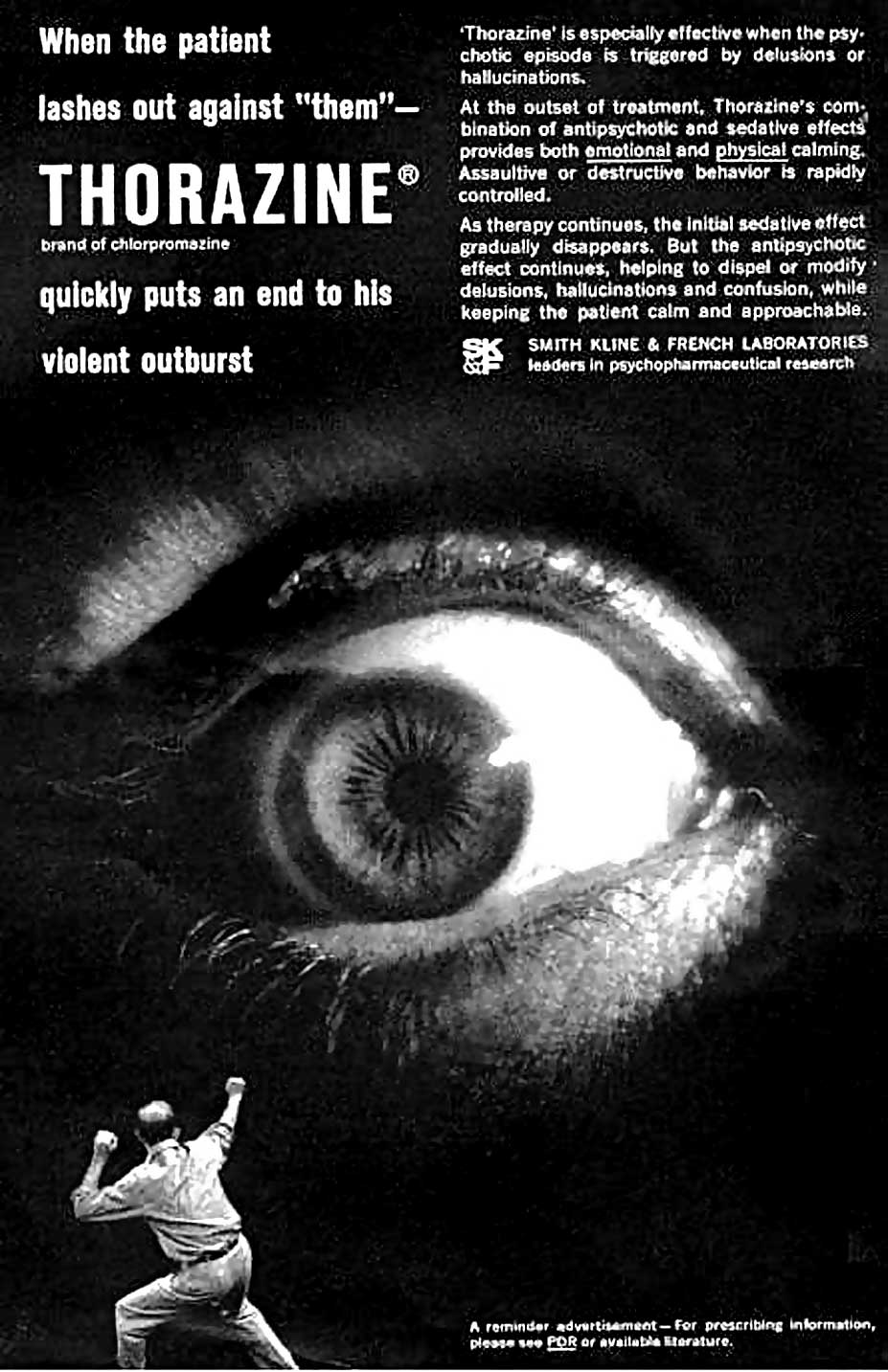 The original antipsychotic drugs were happened upon largely by chance and then tested for their effectiveness. The first, chlorpromazine, was developed as a surgical anesthetic. It was first used on psychiatric patients because of its powerful calming effect; at the time it was regarded as a non-permanent "pharmacological lobotomy".
The original antipsychotic drugs were happened upon largely by chance and then tested for their effectiveness. The first, chlorpromazine, was developed as a surgical anesthetic. It was first used on psychiatric patients because of its powerful calming effect; at the time it was regarded as a non-permanent "pharmacological lobotomy".antidepressant
Antidepressants are a class of medication used to treat major depressive disorder, anxiety disorders, chronic pain conditions, and to help manage addictions. Common side-effects of antidepressants include dry mouth, weight gain, dizziness, hea ...
s, anxiolytics, and the majority of other drugs now used in the management of psychiatric conditions. In 1952, Henri Laborit described chlorpromazine only as inducing indifference towards what was happening around them in nonpsychotic, nonmanic patients, and Jean Delay
Jean Delay (14 November 1907, Bayonne ā 29 May 1987, Paris) was a French psychiatrist, neurologist, writer, and a member of the AcadĆ©mie franƧaise (Chair 17).
His assistant Pierre Deniker conducted a test of chlorpromazine on the male mental ...
and Pierre Deniker
Pierre Deniker (16 February 1917, in Paris ā 17 August 1998) was involved, jointly with Jean Delay and J. M. Harl, in the introduction of chlorpromazine (Thorazine), the first antipsychotic used in the treatment of schizophrenia, in the 1950s. ...
described it as controlling manic or psychotic agitation. The former claimed to have discovered a treatment for agitation in anyone, and the latter team claimed to have discovered a treatment for psychotic illness.
Until the 1970s there was considerable debate within psychiatry on the most appropriate term to use to describe the new drugs.reserpine
Reserpine is a drug that is used for the treatment of high blood pressure, usually in combination with a thiazide diuretic or vasodilator. Large clinical trials have shown that combined treatment with reserpine plus a thiazide diuretic reduces m ...
from the older sedatives. The word ''neuroleptic'' was coined in 1955 by Delay and Deniker after their discovery (1952) of the antipsychotic effects of chlorpromazine.sinew
A tendon or sinew is a tough, high-tensile-strength band of dense fibrous connective tissue that connects muscle to bone. It is able to transmit the mechanical forces of muscle contraction to the skeletal system without sacrificing its ability ...
" but today referring to the nerve
A nerve is an enclosed, cable-like bundle of nerve fibers (called axons) in the peripheral nervous system.
A nerve transmits electrical impulses. It is the basic unit of the peripheral nervous system. A nerve provides a common pathway for the e ...
s) and " Ī»Ī±Ī¼Ī²Ī¬Ī½Ļ" (''lambanÅ'', meaning "take hold of"). Thus, the word means ''taking hold of one's nerves''. It was often taken to refer also to common side effects such as reduced activity in general, as well as lethargy and impaired motor control. Although these effects are unpleasant and in some cases harmful, they were at one time, along with akathisia, considered a reliable sign that the drug was working.neuroses
Neurosis is a class of functional mental disorders involving chronic distress, but neither delusions nor hallucinations. The term is no longer used by the professional psychiatric community in the United States, having been eliminated from th ...
.hypnotic
Hypnotic (from Greek ''Hypnos'', sleep), or soporific drugs, commonly known as sleeping pills, are a class of (and umbrella term for) psychoactive drugs whose primary function is to induce sleep (or surgical anesthesiaWhen used in anesthesia ...
drugs such as the benzodiazepine
Benzodiazepines (BZD, BDZ, BZs), sometimes called "benzos", are a class of depressant drugs whose core chemical structure is the fusion of a benzene ring and a diazepine ring. They are prescribed to treat conditions such as anxiety disorders, ...
s and nonbenzodiazepines, which are useful as generally short-term management for insomnia together with cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. CBT focuses on challenging and changing cognitive distortions (suc ...
for insomnia. They are potentially addictive sedatives.
Antipsychotics are broadly divided into two groups, the typical or first-generation antipsychotics and the atypical or second-generation antipsychotics. The difference between first- and second-generation antipsychotics is a subject of debate. The second-generation antipsychotics are generally distinguishable by the presence of 5HT2A receptor
The 5-HT2A receptor is a subtype of the 5-HT2 receptor that belongs to the serotonin receptor family and is a G protein-coupled receptor (GPCR). The 5-HT2A receptor is a cell surface receptor, but has several intracellular locations. 5-HT is sh ...
antagonism and a corresponding lower propensity for extrapyramidal side effects compared to first-generation antipsychotics.
Society and culture
Terminology
The term ''major tranquilizer'' was used for older antipsychotic drugs. The term ''neuroleptic'' is often used as a synonym
A synonym is a word, morpheme, or phrase that means exactly or nearly the same as another word, morpheme, or phrase in a given language. For example, in the English language, the words ''begin'', ''start'', ''commence'', and ''initiate'' are all ...
for ''antipsychotic'', even though ā strictly speaking ā the two terms are not interchangeable. ''Antipsychotic'' drugs are a subgroup of ''neuroleptic'' drugs, because the latter have a wider range of effects.psychoactive
A psychoactive drug, psychopharmaceutical, psychoactive agent or psychotropic drug is a chemical substance, that changes functions of the nervous system, and results in alterations in perception, mood, consciousness, cognition or behavior.
Th ...
or psychotropic medication.
Sales
Antipsychotics were once among the biggest selling and most profitable of all drugs, generating $22 billion in global sales in 2008.[Pipelineantipsychotic drugs to drive next market evolution (2009)](_blank)
Healthcarefinancenews.com (7 August 2009). By 2003 in the US, an estimated 3.21 million patients received antipsychotics, worth an estimated $2.82 billion. Over 2/3 of prescriptions were for the newer, more expensive atypicals, each costing on average $164 per year, compared to $40 for the older types.
Overprescription
Antipsychotics in the nursing home population are often overprescribed, often for the purposes of making it easier to handle dementia patients. Federal efforts to reduce the use of antipsychotics in US nursing homes has led to a nationwide decrease in their usage in 2012.
Legal
Antipsychotics are sometimes administered as part of compulsory psychiatric treatment via inpatient (hospital) commitment or outpatient commitment.
Formulations
They may be administered orally or, in some cases, through long-acting (depot) injections administered in the dorsgluteal, ventrogluteal
The gluteal muscles, often called glutes are a group of three muscles which make up the gluteal region commonly known as the buttocks: the gluteus maximus, gluteus medius and gluteus minimus. The three muscles originate from the ilium and s ...
or deltoid muscle. Short-acting parenteral formulations also exist, which are generally reserved for emergencies or when oral administration is otherwise impossible. The oral formulations include immediate release, extended release, and orally disintegrating products (which are not sublingual, and can help ensure that medications are swallowed instead of "cheeked"). Sublingual products (e.g. asenapine) also exist, which must be held under the tongue for absorption. The first transdermal formulation of an antipsychotic (transdermal asenapine, marketed as Secuado), was FDA-approved in 2019.
Recreational use
Certain second-generation antipsychotics are misused or abused for their sedative, tranquilizing, and (paradoxically) "hallucinogenic" effects.
Controversy
Joanna Moncrieff has argued that antipsychotic drug treatment is often undertaken as a means of control rather than to treat specific symptoms experienced by the patient.Johnson & Johnson
Johnson & Johnson (J&J) is an American multinational corporation founded in 1886 that develops medical devices, pharmaceuticals, and consumer packaged goods. Its common stock is a component of the Dow Jones Industrial Average and the company i ...
for allegedly paying kickbacks to Omnicare to promote its antipsychotic risperidone (Risperdal) in nursing homes.Eli Lilly and Company
Eli Lilly and Company is an American pharmaceutical company headquartered in Indianapolis, Indiana, with offices in 18 countries. Its products are sold in approximately 125 countries. The company was founded in 1876 by, and named after, Colonel ...
's antipsychotic Zyprexa, and the other involved Bextra
Valdecoxib is a nonsteroidal anti-inflammatory drug (NSAID) used in the treatment of osteoarthritis, rheumatoid arthritis, and painful menstruation and menstrual symptoms. It is a selective cyclooxygenase-2 inhibitor. It was patented in 1995.
...
. In the Bextra case, the government also charged Pfizer with illegally marketing another antipsychotic, Geodon.[ In addition, AstraZeneca faces numerous personal-injury lawsuits from former users of ]Seroquel
Quetiapine, sold under the brand name Seroquel among others, is an atypical antipsychotic medication used for the treatment of schizophrenia, bipolar disorder, and major depressive disorder. Despite being widely used as a sleep aid due to its ...
(quetiapine), amidst federal investigations of its marketing practices.Johnson & Johnson
Johnson & Johnson (J&J) is an American multinational corporation founded in 1886 that develops medical devices, pharmaceuticals, and consumer packaged goods. Its common stock is a component of the Dow Jones Industrial Average and the company i ...
gave more than $700,000 to a research center that was headed by Biederman from 2002 to 2005, where research was conducted, in part, on Risperdal
Risperidone, sold under the brand name Risperdal among others, is an atypical antipsychotic used to treat schizophrenia and bipolar disorder. It is taken either by mouth or by injection (subcutaneous or intramuscular). The injectable versions ...
, the company's antipsychotic drug. Biederman has responded saying that the money did not influence him and that he did not promote a specific diagnosis or treatment.[
Pharmaceutical companies have also been accused of attempting to set the mental health agenda through activities such as funding consumer advocacy groups.]
Special populations
It is recommended that persons with dementia who exhibit behavioral and psychological symptoms should not be given antipsychotics before trying other treatments.[, which cites
*
*
*
*
* ] When taking antipsychotics this population has increased risk of cerebrovascular effects, parkinsonism or extrapyramidal symptoms, sedation, confusion and other cognitive adverse effects, weight gain, and increased mortality.[, which cites
*
*
*
* ]
See also
* List of investigational antipsychotics
* Antipsychotic switching
Notes
References
Further reading
*
External links
Recommendations for the use of antipsychotics for treating psychosis
World Health Organization 2012
Are atypical antipsychotics advantageous? ā the case for
Australian Prescriber 2005 (note: pharmaceutical company conflict of interest statement at the end)
Are atypical antipsychotics advantageous? ā the case against
Australian Prescriber 2005
First Generation Antipsychotics: An Introduction
Psychopharmacology Institute, 2012
ā Public Health Advisory for Antipsychotic Drugs used for Treatment of Behavioral Disorders in Elderly Patients, fda.gov
Antipsychotic Medication
ā information from mental health charity The Royal College of Psychiatrists
*
FROTA LH. ''Fifty Years of Antipsychotic Drugs in Psychiatry. "CinqĆ¼enta Anos de Medicamentos AntipsicĆ³ticos em Psiquiatria."''
1st ed; Ebook: CD-Rom/On-Line Portuguese, , File .pdf (Adobe Acrobat) 6Mb, InformƔtica, Rio de Janeiro, August 2003, 486pp., medicina.ufrj.br
{{Authority control
Psychiatry controversies
Drug classes defined by psychological effects
Dopamine antagonists
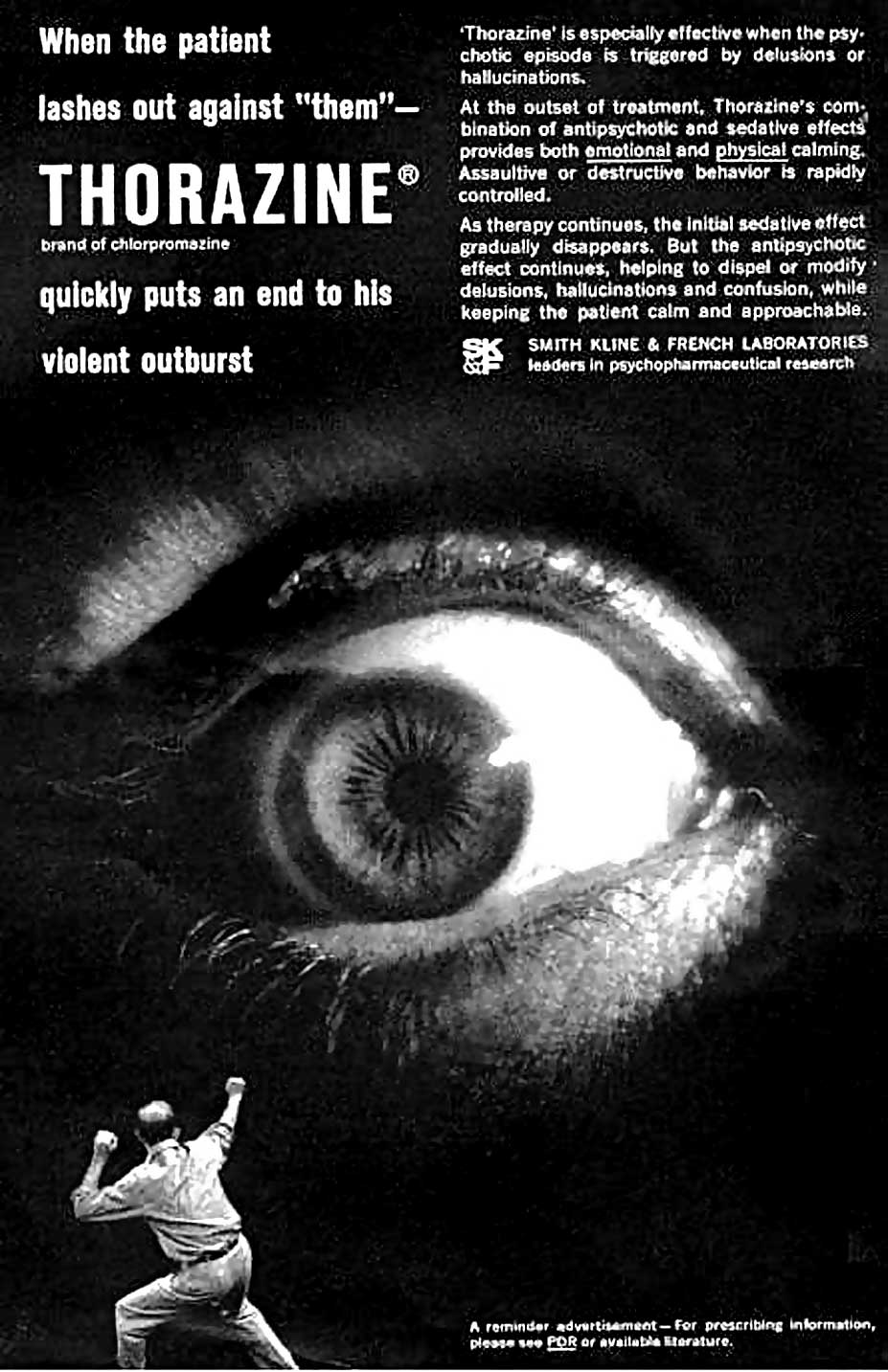 The original antipsychotic drugs were happened upon largely by chance and then tested for their effectiveness. The first, chlorpromazine, was developed as a surgical anesthetic. It was first used on psychiatric patients because of its powerful calming effect; at the time it was regarded as a non-permanent "pharmacological lobotomy". Lobotomy at the time was used to treat many behavioral disorders, including psychosis, although its effect was to markedly reduce behavior and mental functioning of all types. However, chlorpromazine proved to reduce the effects of psychosis in a more effective and specific manner than lobotomy, even though it was known to be capable of causing severe sedation. The underlying neurochemistry involved has since been studied in detail, and subsequent antipsychotic drugs have been developed by rational drug design.
The discovery of chlorpromazine's psychoactive effects in 1952 led to further research that resulted in the development of
The original antipsychotic drugs were happened upon largely by chance and then tested for their effectiveness. The first, chlorpromazine, was developed as a surgical anesthetic. It was first used on psychiatric patients because of its powerful calming effect; at the time it was regarded as a non-permanent "pharmacological lobotomy". Lobotomy at the time was used to treat many behavioral disorders, including psychosis, although its effect was to markedly reduce behavior and mental functioning of all types. However, chlorpromazine proved to reduce the effects of psychosis in a more effective and specific manner than lobotomy, even though it was known to be capable of causing severe sedation. The underlying neurochemistry involved has since been studied in detail, and subsequent antipsychotic drugs have been developed by rational drug design.
The discovery of chlorpromazine's psychoactive effects in 1952 led to further research that resulted in the development of