Angioplasty, Laser on:
[Wikipedia]
[Google]
[Amazon]
Angioplasty, is also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular
 A coronary angioplasty is a therapeutic procedure to treat the
A coronary angioplasty is a therapeutic procedure to treat the

 Access to the vascular system is typically gained percutaneously (through the skin, without a large surgical incision). An introducer sheath is inserted into the blood vessel via the Seldinger technique. Fluoroscopic guidance uses magnetic resonance or X-ray fluoroscopy and radiopaque
Access to the vascular system is typically gained percutaneously (through the skin, without a large surgical incision). An introducer sheath is inserted into the blood vessel via the Seldinger technique. Fluoroscopic guidance uses magnetic resonance or X-ray fluoroscopy and radiopaque
National Heart Lung and Blood Institute, Diseases and Conditions Index
{{authority control Interventional radiology Vascular procedures
procedure
Procedure may refer to:
* Medical procedure
* Instructions or recipes, a set of commands that show how to achieve some result, such as to prepare or make something
* Procedure (business), specifying parts of a business process
* Standard operat ...
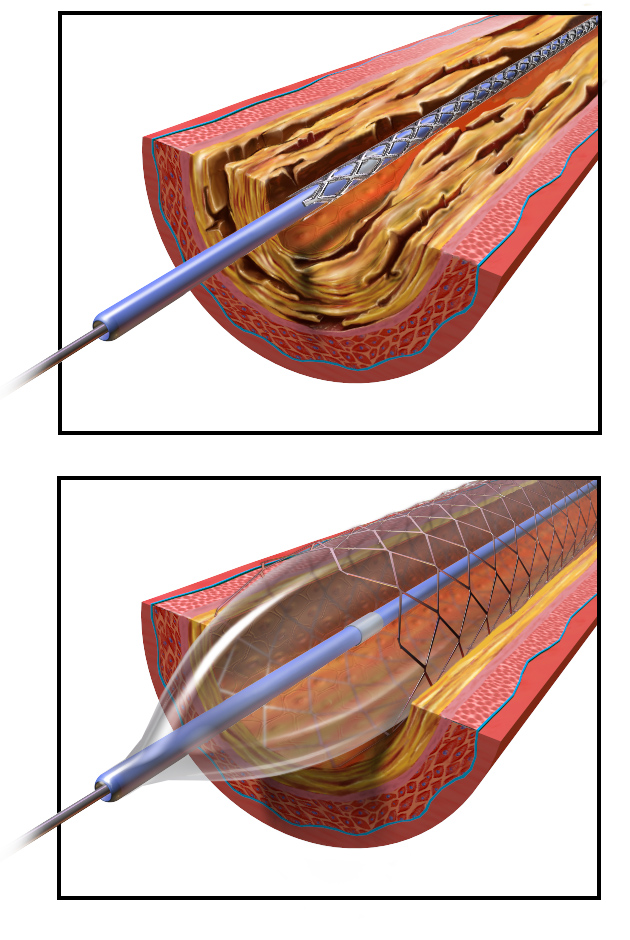
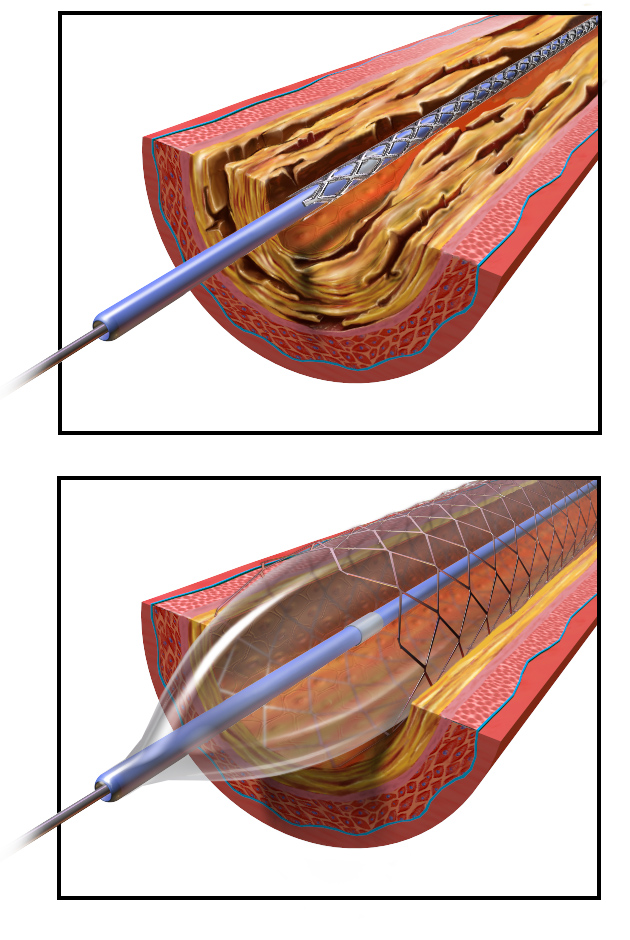
used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis. A deflated balloon attached to a catheter (a balloon catheter) is passed over a guide-wire into the narrowed vessel and then inflated to a fixed size. The balloon forces expansion of the blood vessel and the surrounding muscular wall, allowing an improved blood flow. A stent may be inserted at the time of ballooning to ensure the vessel remains open, and the balloon is then deflated and withdrawn. Angioplasty has come to include all manner of vascular interventions that are typically performed percutaneously.
The word is composed of the combining forms of the Greek words ἀνγεῖον ' "vessel" or "cavity" (of the human body) and πλάσσω ' "form" or "mould".
Uses and indications
Coronary angioplasty
 A coronary angioplasty is a therapeutic procedure to treat the
A coronary angioplasty is a therapeutic procedure to treat the stenotic
A stenosis (from Ancient Greek στενός, "narrow") is an abnormal narrowing in a blood vessel or other tubular organ or structure such as foramina and canals. It is also sometimes called a stricture (as in urethral stricture).
''Stricture'' ...
(narrowed) coronary arteries of the heart found in coronary heart disease. These stenotic segments of the coronary arteries arise due to the buildup of cholesterol-laden plaques that form in a condition known as atherosclerosis. A percutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the ...
(PCI), or coronary angioplasty with stenting, is a non-surgical procedure used to improve the blood flow to the heart.
Coronary angioplasty is indicated for coronary artery disease such as unstable angina, NSTEMI, STEMI and spontaneous coronary artery perforation. PCI for stable coronary disease has been shown to significantly relieve symptoms such as angina
Angina, also known as angina pectoris, is chest pain or pressure, usually caused by ischemia, insufficient blood flow to the Cardiac muscle, heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.
Angina is typical ...
, or chest pain, thereby improving functional limitations and quality of life.
Peripheral angioplasty
Peripheral angioplasty refers to the use of a balloon to open a blood vessel outside the coronary arteries. It is most commonly done to treat atherosclerotic narrowings of the abdomen, leg and renal arteries caused by peripheral artery disease. Often, peripheral angioplasty is used in conjunction with guide wire, peripheralstenting
In medicine, a stent is a metal or plastic tube inserted into the lumen of an anatomic vessel or duct to keep the passageway open, and stenting is the placement of a stent. A wide variety of stents are used for different purposes, from expandab ...
and an atherectomy.
Chronic limb-threatening ischemia
Angioplasty can be used to treat advanced peripheral artery disease to relieve the claudication, or leg pain, that is classically associated with the condition. The bypass versus angioplasty in severe ischemia of the leg (BASIL) trial investigated infrainguinal bypass surgery first compared to angioplasty first in select patients with severe lower limb ischemia who were candidates for either procedure. The BASIL trial found that angioplasty was associated with less short term morbidity compared with bypass surgery, however long term outcomes favor bypass surgery. Based on the BASIL trial, the ACCF/AHA guidelines recommend balloon angioplasty only for patients with a life expectancy of 2 years or less or those who do not have an autogenous vein available. For patients with a life expectancy greater than 2 of years life, or who have an autogenous vein, a bypass surgery could be performed first.Renal artery angioplasty
Renal artery stenosis is associated withhypertension
Hypertension (HTN or HT), also known as high blood pressure (HBP), is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms. Long-term high bl ...
and loss of renal function
Assessment of kidney function occurs in different ways, using the presence of symptoms and signs, as well as measurements using urine tests, blood tests, and medical imaging.
Functions of a healthy kidney include maintaining a person's fluid ...
. Atherosclerotic obstruction of the renal artery can be treated with angioplasty with or without stenting of the renal artery. There is a weak recommendation for renal artery angioplasty in patients with renal artery stenosis and flash edema or congestive heart failure.
Carotid angioplasty
Carotid artery stenosis can be treated with angioplasty and carotid stenting for patients at high risk for undergoing carotid endarterectomy (CEA). Although carotid endarterectomy is typically preferred over carotid artery stenting, stenting is indicated in select patients with radiation-induced stenosis or a carotid lesion not suitable for surgery.Venous angioplasty
Angioplasty is used to treat venous stenosis affecting hemodialysis access, with drug-coated balloon angioplasty proving to have better 6 month and 12 month patency than conventional balloon angioplasty. Angioplasty is occasionally used to treat residualsubclavian vein
The subclavian vein is a paired large vein, one on either side of the body, that is responsible for draining blood from the upper extremities, allowing this blood to return to the heart. The left subclavian vein plays a key role in the absorption ...
stenosis following thoracic outlet decompression
The thorax or chest is a part of the anatomy of humans, mammals, and other tetrapod animals located between the neck and the abdomen. In insects, crustaceans, and the extinct trilobites, the thorax is one of the three main divisions of the crea ...
surgery for thoracic outlet syndrome. There is a weak recommendation for deep venous stenting to treat obstructive chronic venous disease.
Contraindications
Angioplasty requires an access vessel, typically the femoral or radial artery or femoral vein, to permit access to the vascular system for the wires and catheters used. If no access vessel of sufficient size and quality is available, angioplasty is contraindicated. A small vessel diameter, the presence of posterior calcification, occlusion, hematoma, or an earlier placement of a bypass origin, may make access to the vascular system too difficult. Percutaneous transluminal coronary angioplasty (PTCA) is contraindicated in patients with left main coronary artery disease, due to the risk of spasm of the left main coronary artery during the procedure. Also, PTCA is not recommended if there is less than 70% stenosis of the coronary arteries, as the stenosis it is not deemed to be hemodynamically significant below this level.Technique

 Access to the vascular system is typically gained percutaneously (through the skin, without a large surgical incision). An introducer sheath is inserted into the blood vessel via the Seldinger technique. Fluoroscopic guidance uses magnetic resonance or X-ray fluoroscopy and radiopaque
Access to the vascular system is typically gained percutaneously (through the skin, without a large surgical incision). An introducer sheath is inserted into the blood vessel via the Seldinger technique. Fluoroscopic guidance uses magnetic resonance or X-ray fluoroscopy and radiopaque contrast dye
Radiocontrast agents are substances used to enhance the visibility of internal structures in X-ray-based imaging techniques such as computed tomography (contrast CT), projectional radiography, and fluoroscopy. Radiocontrast agents are typically io ...
to guide angled wires and catheters to the region of the body to be treated in real time. Tapered guidewire is chosen for small occlusion, followed by intermediate type guidewires for tortuous arteries and difficulty passing through extremely narrow channels, and stiff wires for hard, dense, and blunt occlusions. To treat a narrowing in a blood vessel, a wire is passed through the stenosis
A stenosis (from Ancient Greek στενός, "narrow") is an abnormal narrowing in a blood vessel or other tubular organ or structure such as foramina and canals. It is also sometimes called a stricture (as in urethral stricture).
''Stricture'' ...
in the vessel and a balloon on a catheter is passed over the wire and into the desired position. The positioning is verified by fluoroscopy and the balloon is inflated using water mixed with contrast dye to 75 to 500 times normal blood pressure
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" r ...
(6 to 20 atmospheres), with most coronary angioplasties requiring less than 10 atmospheres. A stent may or may not also be placed.
At the conclusion of the procedure, the balloons, wires and catheters are removed and the vessel puncture site is treated either with direct pressure or a vascular closure device Vascular closure devices (VCDs) are medical devices used to achieve hemostasis of the small hole in the artery after a cardiovascular procedure of endovascular surgery requiring a catheterization.
Cardiovascular procedures requiring catheterizatio ...
.
Transradial artery access (TRA) and transfemoral artery access (TFA) are two techniques for percutaneous coronary intervention. TRA is the technique of choice for management of acute coronary syndrome (ACS) as it has significantly lower incidence of bleeding and vascular complications compared with the TFA approach. TRA also has a mortality benefit for high risk ACS patients and high risk bleeding patients. TRA was also found to yield improved quality of life, as well as decreased healthcare costs and resources.
Risks and complications
Relative tosurgery
Surgery ''cheirourgikē'' (composed of χείρ, "hand", and ἔργον, "work"), via la, chirurgiae, meaning "hand work". is a medical specialty that uses operative manual and instrumental techniques on a person to investigate or treat a pat ...
, angioplasty is a lower-risk option for the treatment of the conditions for which it is used, but there are unique and potentially dangerous risks and complications associated with angioplasty:
* Embolization, or the launching of debris into the bloodstream
* Bleeding from over-inflation of a balloon catheter or the use of an inappropriately large or stiff balloon, or the presence of a calcified target vessel.
* Hematoma
A hematoma, also spelled haematoma, or blood suffusion is a localized bleeding outside of blood vessels, due to either disease or trauma including injury or surgery and may involve blood continuing to seep from broken capillary, capillaries. A he ...
or pseudoaneurysm formation at the access site
* Radiation-induced injuries (burns) from the X-rays used
* Contrast-induced renal injury
* Cerebral Hyperperfusion Syndrome leading to stroke is a serious complication of carotid artery angioplasty with stenting.
Angioplasty may also provide a less durable treatment for atherosclerosis and be more prone to restenosis relative to vascular bypass or coronary artery bypass grafting. Drug-eluting balloon angioplasty has significantly less restenosis, late lumen loss and target lesion revascularization at both short term and midterm follow-up compared to uncoated balloon angioplasty for femoropopliteal arterial occlusive disease. Although angioplasty of the femoropopliteal artery with paclitaxel-coated stents and balloons significantly reduces rates of vessel restenosis and target lesion revascularization, it was also found to have increased risk of death.
Recovery
After angioplasty, most patients are monitored overnight in the hospital, but if there are no complications, patients are sent home the following day. The catheter site is checked for bleeding and swelling and the heart rate and blood pressure are monitored to detect late rupture and hemorrhage. Post-procedure protocol also involves monitoring urinary output, cardiac symptoms, pain and other signs of systemic problems. Usually, patients receive medication that will relax them to protect the arteries against spasms. Patients are typically able to walk within two to six hours following the procedure and return to their normal routine by the following week. Angioplasty recovery consists of avoiding physical activity for several days after the procedure. Patients are advised to avoid heavy lifting and strenuous activities for a week. Page last reviewed: 28/08/2018 Patients will need to avoid physical stress or prolonged sport activities for a maximum of two weeks after a delicate balloon angioplasty. After the initial two week recovery phase, most angioplasty patients can begin to safely return to low-level exercise. A graduated exercise program is recommended whereby patients initially perform several short bouts of exercise each day, progressively increasing to one or two longer bouts of exercise. As a precaution, all structured exercise should be cleared by a cardiologist before commencing. Exercise-based rehabilitation following percutaneous coronary intervention has shown improvement in recurrent angina, total exercise time, ST-segment decline, and maximum exercise tolerance. Patients who experience swelling, bleeding or pain at the insertion site, develop fever, feel faint or weak, notice a change in temperature or color in the arm or leg that was used or have shortness of breath or chest pain should immediately seek medical advice. Patients with stents are usually prescribed dual antiplatelet therapy (DAPT) which consists of a P2Y12 inhibitor, such as clopidogrel, which is taken at the same time as acetylsalicylic acid (aspirin). Dual antiplatelet therapy (DAPT) is recommended for 1 month following bare metal stent placement, for 3 months following a second generation drug-eluting stent placement, and for 6–12 months following a first generation drug-eluting stent placement. DAPT's antiplatelet properties are intended to prevent blood clots, however they also increase the risk of bleeding, so it is important to consider each patient's preferences, cardiac conditions, and bleeding risk when determining the duration of DAPT treatment. Another important consideration is that concomitant use of Clopidogrel and Proton Pump Inhibitors following coronary angiography is associated with significantly higher adverse cardiovascular complications such as major adverse cardiovascular events (MACE), stent thrombosis and myocardial infarction.History
Angioplasty was first described by the US interventional radiologist Charles Dotter in 1964. Dr. Dotter pioneered modern medicine with the invention of angioplasty and the catheter-delivered stent, which were first used to treat peripheral arterial disease. On January 16, 1964, Dotter percutaneously dilated a tight, localized stenosis of thesubsartorial artery
The femoral artery is a large artery in the thigh and the main arterial supply to the thigh and leg. The femoral artery gives off the deep femoral artery or profunda femoris artery and descends along the anteromedial part of the thigh in the fem ...
in an 82-year-old woman with painful leg ischemia and gangrene who refused leg amputation. After successful dilation of the stenosis with a guide wire and coaxial Teflon catheters, the circulation returned to her leg. The dilated artery stayed open until her death from pneumonia two and a half years later. Charles Dotter is commonly known as the "Father of Interventional Radiology
Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs bo ...
" and was nominated for the Nobel Prize in medicine in 1978.
The first percutaneous coronary angioplasty on an awake patient was performed in Zurich by the German cardiologist Andreas Gruentzig on September 16, 1977.
Dr. Simon H. Stertzer was the first to perform coronary angioplasty in the United States on March 1, 1978, at Lenox Hill Hospital in New York. That same day, Dr. Richard K. Myler of St. Mary's Hospital in San Francisco performed the second coronary angioplasty in the United States.
The initial form of angioplasty was 'plain old balloon angioplasty' (POBA) without stenting, until the invention of bare metal stenting in the mid-1980s to prevent the early restenosis observed with POBA.
Bare metal stents were found to cause in-stent restenosis as a result of neointimal hyperplasia and stent thrombosis, which led to the invention of drug-eluting stents with anti-proliferative drugs to combat in-stent restenosis.
The first coronary angioplasty with a drug delivery stent system was performed by Dr. Stertzer and Dr. Luis de la Fuente, at the Instituto Argentino de Diagnóstico y Tratamiento (English: Argentina Institute of Diagnosis and Treatment) in Buenos Aires, in 1999.
Ingemar Henry Lundquist
Ingemar Henry Lundquist (October 19, 1921 – February 25, 2007) was a prolific inventor and mechanical engineer.
Early life and education
Lundquist graduated from the Stockholm Institute of Technology in 1945 with a mechanical engineering ...
invented the over-the-wire balloon catheter that is now used in the majority of angioplasty procedures in the world.
References
External links
National Heart Lung and Blood Institute, Diseases and Conditions Index
{{authority control Interventional radiology Vascular procedures