4 Hour Targets on:
[Wikipedia]
[Google]
[Amazon]
NHS targets are performance measures used by
 A four-hour target in emergency departments was introduced by the
A four-hour target in emergency departments was introduced by the
/ref> 48% of departments said they did not meet the target for the period ending 31 December 2004.BMA - BMA survey of accident and emergency waiting times, March 2005
/ref> Government figures show that in 2005–06, 98.2% of patients were seen, diagnosed and treated within four hours of their arrival at A&E, the first full financial year in which this has happened. The four-hour target triggered the introduction of the
 By December 2014, the number of patients being treated within four hours had fallen to 91.8%. From December 2015, the 95% target over England as a whole was missed every month. From October–December 2016, only 4 out of 139 hospitals with major type 1 A&E departments met the target. In November 2018, the
By December 2014, the number of patients being treated within four hours had fallen to 91.8%. From December 2015, the 95% target over England as a whole was missed every month. From October–December 2016, only 4 out of 139 hospitals with major type 1 A&E departments met the target. In November 2018, the
NHS England
NHS England, officially the NHS Commissioning Board, is an executive non-departmental public body of the Department of Health and Social Care. It oversees the budget, planning, delivery and day-to-day operation of the commissioning side of the ...
, NHS Scotland
NHS Scotland, sometimes styled NHSScotland, is the publicly funded healthcare system in Scotland and one of the four systems that make up the National Health Service in the United Kingdom. It operates 14 territorial NHS boards across Scotland, ...
, NHS Wales
NHS Wales ( cy, GIG (Gwasanaeth Iechyd Gwladol) Cymru) is the publicly-funded healthcare system in Wales, and one of the four systems which make up the National Health Service in the United Kingdom.
NHS Wales was formed as part of the public ...
, and the Health and Social Care service in Northern Ireland. These vary by country but assess the performance of each health service against measures such as 5 hour waiting times in Accident and Emergency departments, weeks to receive an appointment and/or treatment, and performance in specific departments such as oncology
Oncology is a branch of medicine that deals with the study, treatment, diagnosis and prevention of cancer. A medical professional who practices oncology is an ''oncologist''. The name's etymological origin is the Greek word ὄγκος (''ó ...
.
History
TheMajor
Major (commandant in certain jurisdictions) is a military rank of commissioned officer status, with corresponding ranks existing in many military forces throughout the world. When used unhyphenated and in conjunction with no other indicators ...
Conservative government first set public targets for the NHS
The National Health Service (NHS) is the umbrella term for the publicly funded healthcare systems of the United Kingdom (UK). Since 1948, they have been funded out of general taxation. There are three systems which are referred to using the " ...
in the 1990s – for example, guaranteeing a maximum two-year wait for non-emergency surgery and reducing rates of death from specific diseases.
The subsequent Labour government introduced far more targets and managed performance far more aggressively - a management regime sometimes referred to as 'targets and terror'. Targets were blamed for distorting clinical priorities, and in particular for one organisation achieving a target at the expense of another. For example, ambulances have been forced to queue up outside a busy emergency departments so that the ambulances might not be able to meet their target in responding to emergency calls, but the hospital can meet its A&E target. Excess emphasis on the targets can mean that other important aspects of care, especially those not easily measured, may be neglected. Some have however praised targets for producing faster reductions in waiting times in England than other UK countries between 1996 and 2006.
NHS England
NHS England, officially the NHS Commissioning Board, is an executive non-departmental public body of the Department of Health and Social Care. It oversees the budget, planning, delivery and day-to-day operation of the commissioning side of the ...
under the Conservative governments reduced the number of targets, in particular removing most of those relating to health inequality, and encouraged a system wide approach. However shortage of staff and funding meant that performance against targets nonetheless declined. Guidance published in February 2018 conceded that most of the targets would not be met before April 2019. The hospital care and A&E performance measures for October 2019 were the worst ever recorded.
Sajid Javid called for a ‘proper review of NHS targets’ in September 2021.
According to Jeremy Hunt
Jeremy Richard Streynsham Hunt (born 1 November 1966) is a British politician who has served as Chancellor of the Exchequer since 14 October 2022. He previously served in the Cabinet as Secretary of State for Culture, Olympics, Media and Sport ...
the Stafford Hospital scandal
The Stafford Hospital scandal concerns poor care and high mortality rates amongst patients at the Stafford Hospital, Stafford, England, during the first decade of the 21st century. The hospital was run by the Mid Staffordshire NHS Foundation Trust ...
showed that concentrating on national targets led to managers deprioritising the safety and well-being of patients. Targets can benefit patients but they can also lead to bureaucracy, gaming and poor patient care, or as David Nicholson famously put it - "hitting the target and missing the point". But they are alluring to politicians. Hunt says the effectiveness of targets is in inverse proportion to their quantity and points out that no other country runs its healthcare system by targets. Goodhart's law
Goodhart's law is an adage often stated as, "When a measure becomes a target, it ceases to be a good measure". It is named after British economist Charles Goodhart, who is credited with expressing the core idea of the adage in a 1975 article on mon ...
applies: "When a measure becomes a target, it ceases to be a good measure".
National approaches
England
The NHS Constitution for England specifies waiting times in the accompanying Handbook, but does not provide a remedy should they be breached. Non-acute crisis response waiting time targets are to be introduced byNHS England
NHS England, officially the NHS Commissioning Board, is an executive non-departmental public body of the Department of Health and Social Care. It oversees the budget, planning, delivery and day-to-day operation of the commissioning side of the ...
for integrated care system
In England, an integrated care system (ICS) is a statutory partnership of organisations who plan, buy, and provide health and care services in their geographical area. The organisations involved include the NHS, local authorities, voluntary and cha ...
s from April 2022. Performance is to be measured on the percentage of services delivered within two hours. Mental health targets are also planned, although no start date has been set, requiring require that urgent referrals to community crisis services should be seen within 24 hours, and “very urgent” referrals should be seen within four hours. Mental health patients referred from emergency departments should be seen face-to-face by liaison teams within one hour.
Scotland
ThePatient Rights (Scotland) Act 2011
The Patient Rights (Scotland) Act 2011 is an Act of the Scottish Parliament.
The Act states that healthcare providers must consider the needs of patients, consider what would be the most beneficial to the patient, taking into account their circu ...
establishes the treatment time guarantee, but also does not specify a remedy should it not be met.
Northern Ireland
Targets in Northern Ireland are set by theHealth and Social Care Board
The Health and Social Care Board is an organisation responsible for the commissioning of health services for the people of Northern Ireland. Its current chief executive is Ms. Valerie Watts.
Creation
The Health and Social Care (Reform) Act (Nor ...
and are less demanding than in the rest of the UK. None have been met since 2015, and some for considerably longer.
Wales
Targets in Wales are set by the Welsh Government and set out in the NHS Wales Delivery Framework. The Welsh Government has taken a different approach to some areas of care, such as becoming the first nation in the UK to have a single waiting times target for cancer treatment. The Welsh NHS has broadly under-performed compared to the English NHS, with higher waiting times for both urgent and routine care. However aFull Fact
Full Fact is a British charity, based in London, which checks and corrects facts reported in the news as well as claims which circulate on social media.
History and structure
Full Fact was founded in 2009 by businessman Michael Samuel, the c ...
report by the Chief Executive of the Nuffield Trust Nigel Edwards acknowledges that the two nations targets are not directly comparable because "the Welsh population is older, sicker and more deprived than the English population—so its NHS has to work harder".
Accident and emergency departments
 A four-hour target in emergency departments was introduced by the
A four-hour target in emergency departments was introduced by the Department of Health
A health department or health ministry is a part of government which focuses on issues related to the general health of the citizenry. Subnational entities, such as states, counties and cities, often also operate a health department of their ow ...
for National Health Service
The National Health Service (NHS) is the umbrella term for the publicly funded healthcare systems of the United Kingdom (UK). Since 1948, they have been funded out of general taxation. There are three systems which are referred to using the " ...
acute
Acute may refer to:
Science and technology
* Acute angle
** Acute triangle
** Acute, a leaf shape in the glossary of leaf morphology
* Acute (medicine), a disease that it is of short duration and of recent onset.
** Acute toxicity, the adverse eff ...
hospitals
A hospital is a health care institution providing patient treatment with specialized health science and auxiliary healthcare staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emerge ...
in England
England is a country that is part of the United Kingdom. It shares land borders with Wales to its west and Scotland to its north. The Irish Sea lies northwest and the Celtic Sea to the southwest. It is separated from continental Europe b ...
. The original target was set at 100%, but lowered to reflect clinical concerns that there will always be patients who need to spend slightly longer in A&E, under observation. Setting a target that, by 2004, at least 98% of patients attending an A&E department must be seen, treated, and admitted or discharged in under four hours. The target was further moved to 95% of patients within four hours in 2010 as a result of the coalition's claims that 98% was not clinically justified. Trusts which failed to meet the target could be fined. In July 2016 NHS trusts were set new "performance improvement trajectories". For 47 of the 140 trusts with "type one" major A&E facilities this meant a target of less than 95% waiting under 4 hours. In January 2017 Jeremy Hunt
Jeremy Richard Streynsham Hunt (born 1 November 1966) is a British politician who has served as Chancellor of the Exchequer since 14 October 2022. He previously served in the Cabinet as Secretary of State for Culture, Olympics, Media and Sport ...
announced that the target would in future only apply to "urgent health problems". In January 2018 only 77.1% of patients were admitted or discharged within four hours, the worst ever performance for type one A&E departments. In December 2018 it was reported that patients with only minor ailments could be excluded from the target and a new target introduced so the most urgent cases should be seen within an hour.
The effect of the target can be that patients waiting just below 4 hours get a lot of attention, but once the target is breached there is no further consequence. The average time spent by a patient in A&E who has breached four hours is around eight hours.
In January 2022 research published in the British Medical Journal
''The BMJ'' is a weekly peer-reviewed medical trade journal, published by the trade union the British Medical Association (BMA). ''The BMJ'' has editorial freedom from the BMA. It is one of the world's oldest general medical journals. Origi ...
found that there was one extra death For every 82 admitted patients whose time to inpatient bed transfer is delayed more than 6 to 8 hours from time of arrival at the emergency department.
New standards
In May 2021, after prolonged consultationNHS England
NHS England, officially the NHS Commissioning Board, is an executive non-departmental public body of the Department of Health and Social Care. It oversees the budget, planning, delivery and day-to-day operation of the commissioning side of the ...
announced that the 4 hour target was to be replaced by a new set of 10 metrics. The new “bundle of ten standards” includes
*Response times for ambulances
*Reducing avoidable trips (conveyance rates) to emergency departments by 999 ambulances
*Proportion of contacts via NHS 111
111 is a free-to-call single non-emergency number medical helpline operating in England, Scotland and parts of Wales. The 111 phone service has replaced the various non-geographic 0845 rate numbers and is part of each country's National Health S ...
that receive clinical input
*Percentage of ambulance handovers (from ambulance to A&E) within 15 minutes
*Time to initial assessment — percentage within 15 minutes
*Average time in department — for non-admitted patients
*Average time in department — for admitted patients
*Clinically ready to proceed (time from when decision is made to admit or discharge, and patient is admitted or discharged)
*Patients spending more than 12 hours in A&E
*Critical time standards — aimed at ensuring the highest priority patients get care within a set timeframe such as an hour
In September 2022 Thérèse Coffey
Thérèse Anne Coffey (born 18 November 1971) is a British politician who has served as Secretary of State for Environment, Food and Rural Affairs since October 2022. A member of the Conservative Party, she previously served as Deputy Prime Mini ...
said: “I can absolutely say there will be no changes to the target for four-hour waits in A&E.”
Objective
TheLabour
Labour or labor may refer to:
* Childbirth, the delivery of a baby
* Labour (human activity), or work
** Manual labour, physical work
** Wage labour, a socioeconomic relationship between a worker and an employer
** Organized labour and the labour ...
government (1997-2010) had identified a requirement to promote improvements in A&E departments, which had suffered under-funding for a number of years. The target, accompanied by extra financial support, was a key plan to achieve the improvements. Prime Minister Blair felt the targets had been successful in achieving their aim. "We feel, and maybe we are wrong, that one way we've managed to do that promote improvements in A&E is by setting a clear target".BBC NEWS , Health , Target 'putting A&E care at risk'/ref> 48% of departments said they did not meet the target for the period ending 31 December 2004.BMA - BMA survey of accident and emergency waiting times, March 2005
/ref> Government figures show that in 2005–06, 98.2% of patients were seen, diagnosed and treated within four hours of their arrival at A&E, the first full financial year in which this has happened. The four-hour target triggered the introduction of the
acute assessment unit An acute admissions unit is a short-stay department in some British, Australian and New Zealand hospitals that may be linked to the emergency department, but functions as a separate department.
The AMU acts as a gateway between a patient's gener ...
(also known as the medical assessment unit), which works alongside the emergency department but is outside it for statistical purposes in the bed management
Bed management is the allocation and provision of beds, especially in a hospital where beds in specialist wards are a scarce resource. The "bed" in this context represents not simply a place for the patient to sleep, but the services that go wit ...
cycle. It is claimed that though A&E targets have resulted in significant improvements in completion times, the current target would not have been possible without some form of patient re-designation or re-labelling taking place, so true improvements are somewhat less than headline figures might suggest and it is doubtful that a single target (fitting all A&E and related services) is sustainable.
Although the four-hour target helped to bring down waiting times when it was first introduced, since September 2012 (after the introduction of the Health and Social Care Act 2012
The Health and Social Care Act 2012c 7 is an act of the Parliament of the United Kingdom. It provided for the most extensive reorganisation of the structure of the National Health Service in England to date.''BMJ'', 2011; 342:d408Dr Lansley's Mon ...
and top-down reorganisation of the NHS) hospitals in England struggled to stick to it, prompting suggestions that A&E departments may be reaching a limit in terms of what can be achieved within the available resources. The announcement of the reduction of the target from 98% to 95% was immediately followed by a reduction in attainment to the lower level.
Performance
 By December 2014, the number of patients being treated within four hours had fallen to 91.8%. From December 2015, the 95% target over England as a whole was missed every month. From October–December 2016, only 4 out of 139 hospitals with major type 1 A&E departments met the target. In November 2018, the
By December 2014, the number of patients being treated within four hours had fallen to 91.8%. From December 2015, the 95% target over England as a whole was missed every month. From October–December 2016, only 4 out of 139 hospitals with major type 1 A&E departments met the target. In November 2018, the British Medical Association
The British Medical Association (BMA) is a registered trade union for doctors in the United Kingdom. The association does not regulate or certify doctors, a responsibility which lies with the General Medical Council. The association's headquar ...
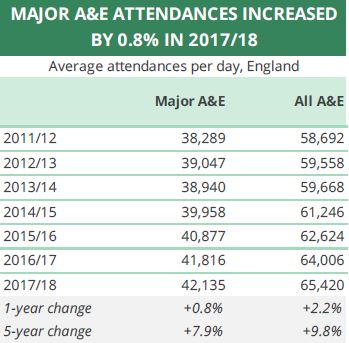
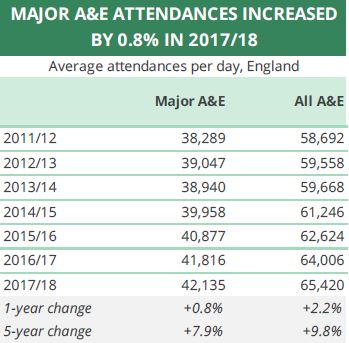
reported that performance on emergency admissions, trolley waits for more than four hours and A&E patients seen within four hours in the summer of 2017 was worse than in the winters of 2011–15. Performance against the four-hour wait target in the summer of 2018 was the worst second quarter performance recorded. Only 88.9% of patients were seen within four hours in September. The number of people admitted, transferred or discharged within four hours in emergency departments in September was up more than 3% compared to September 2017 with a 7% rise in emergency admissions said by John Appleby to be astonishing. Attendance at A&E departments has been increasingly steadily for many years, more so at ‘type 3’ departments, like urgent care centres (where waiting times are generally lower). In the first eight months of 2018, an average of 67,000 people attended each day. In January 2019, only 84.4% of patients were seen within four hours, the worst figure since the target was introduced in 2004. In November 2019 not a single A&E department hit the four-hour wait time target.
Performance in the first three months of 2019-20 was the worst since records began in 2011.
National A&E performance
Scotland
In Scotland, the target is for 95% of A&E patients to be either admitted, transferred or discharged in four hours. It was last met in July 2017. Scotland has performed best on this measure out of the four UK nations, a position it has held since September 2015. However like all other UK nations this performance has recently declined. In Scotland this target has dropped 5% between May 2018 and September 2019.England
In England, the target is also for 95% of A&E patients to be treated, transferred, and discharged within four hours. However performance has fluctuated between 90 and 84% between 2015 and 2019, consistently putting it second in the United Kingdom. However performance against the target declined almost 10% between May 2018 and September 2019. In March 2022 average waits for an ambulance for stroke and heart attack patients (category 2) reached as long as two hours in some regions. The national target for reaching them is 18 minutes. According to the Association of Ambulance Chief Executives more than 3,000 patients may have suffered “severe harm” from ambulance delays in February 2022. In June 2022 ambulance response times for the most serious category one incidents, including cardiac arrests, sank to an average of 9 minutes and 6 seconds, half a minute slower than in May. The target time is 7 minutes.Maria Caulfield
Maria Colette Caulfield (born 6 August 1973) is a British politician and nurse serving as Parliamentary Under Secretary of State for Mental Health and Women’s Health Strategy and Parliamentary Under-Secretary of State for Women since October ...
told the House of Commons on 10 July 2022 that ambulance service response time performance had improved month on month, but in fact it had deteriorated in June.
Wales
In Wales, the target is also for 95% of A&E patients to be treated, transferred, and discharged within four hours. While higher than the performance in Northern Ireland (60%), the Welsh NHS is third in the United Kingdom, putting it 7 percent behind NHS England and 8% behind NHS Scotland. The Nuffield Trust have identified Welsh underperformance as influenced by the Welsh population being older, sicker and having more deprivation than any other UK nation. Performance against the target has like all other UK nations in recent years, having declined by 7.5% between May 2018 and September 2019.Northern Ireland
Targets in Northern Ireland are set by theHealth and Social Care Board
The Health and Social Care Board is an organisation responsible for the commissioning of health services for the people of Northern Ireland. Its current chief executive is Ms. Valerie Watts.
Creation
The Health and Social Care (Reform) Act (Nor ...
and are less demanding than in the rest of the UK. None have been met since 2015, and some for considerably longer. A&E waits when considered using the NHS measure of 4 hours to discharge show that performance in Northern Ireland has dropped 13% between May 2018 and September 2019.
Missing the target
According to the BMA the main reasons for not reaching this target are: *Not enoughinpatient
A patient is any recipient of health care services that are performed by healthcare professionals. The patient is most often ill or injured and in need of treatment by a physician, nurse, optometrist, dentist, veterinarian, or other health ca ...
beds
*Delayed discharges
*Delay in accessing specialist opinion
*Not enough nurses
*Not enough middle grade doctors
*Department too small
*Delay in accessing diagnostic services
In 2014, research conducted by QualityWatch, a joint programme from the Nuffield Trust
The Nuffield Trust, formerly the Nuffield Provincial Hospitals Trust, is a charitable trust with the mission of improving health care in the UK through evidence and analysis.
The Nuffield Trust is registered with the Charity Commission as char ...
and the Health Foundation
The Health Foundation is an independent charity for health care for people in the UK.
The organisation’s aim is a healthier population, supported by high quality health care that can be equitably accessed. Its programs include making grants to ...
, tracked 41 million visits to A&E departments in England in order to better understand the pressures leading to increased waiting times and breaches of the four-hour target. Researchers identified a rise in older patients and related increase in long-term conditions as key factors, alongside extremes of temperature (in both summer and winter) and crowding at peak times. They noted that the majority of pressure was falling on major A&E units, and proposed that rising demand as a result of ageing and population growth may be pushing already stretched emergency departments beyond maximum capacity.
In July 2017 the Royal College of Emergency Medicine
The Royal College of Emergency Medicine (RCEM) is an independent professional association of emergency physicians in the United Kingdom which sets standards of training and administers examinations for emergency medicine. The patron is The Princ ...
produced a report saying that the NHS needed at least 5,000 more beds to achieve safe bed occupancy levels and hit the four-hour target.
Pressure
Even though exceptions are allowed to the targets, concerns have been raised that the target has put pressure on A&E staff to compromise patient care. A significant proportion (90%) of A&E consultants welcomed the four hour target in a study but felt that 98% was too high a target.Twelve hour target
England
At the same time as the four target was introduced a target that no patient should wait longer than 12 hours before they are admitted to a ward, if that is required, was introduced. In England time was measured from the point a decision to admit is made and not from the moment the patient arrives. Between January and March 2012 only 15 patients in England waited more than 12 hours, but in the same months in 2017 1,597 patients breached the target. In January 2018 1,043 patients waited over 12 hours for a bed, the worst figure ever recorded. 272 were atUniversity Hospitals of North Midlands NHS Trust
The University Hospitals of North Midlands NHS Trust was created on 1 November 2014. It runs Royal Stoke University Hospital, formerly run by the University Hospital of North Staffordshire NHS Trust and the County Hospital (formerly Stafford Hosp ...
. Problems at Lancashire Care NHS Foundation Trust
Lancashire & South Cumbria NHS Foundation Trust, known as Lancashire Care NHS Foundation Trust until October 2019, provides a range of services including secondary mental health care, inpatient child and adolescent mental health services, perin ...
led to more than 1,000 cases of patients waiting over 12 hours for admission in 2018–19. This was about a third of all the 12 hour breaches, which were mostly mental health cases - where admission to a ward is not within the control of the trust running the A&E department. A review found that some patients in Lancashire were “potentially being held against their will without appropriate legal provision”. Some were detained in seclusion rooms for more than a week under section 136 of the Mental Health Act 1983
The Mental Health Act 1983 (c.20) is an Act of the Parliament of the United Kingdom. It covers the reception, care and treatment of mentally disordered people, the management of their property and other related matters, forming part of the ment ...
, which only provides that patients can be lawfully detained for 24 hours, with a possible 12-hour extension. In December 2019 trusts in London were told to set up dedicated spaces to care for three mental health patients in every A&E department.
In December 2019 there were 2,347 breaches, compared with 284 recorded in December 2018. In February 2022 there were 16,404 breaches and in March 2022 22,506. The NHS Standard Contract for 2022-23 requires hospitals to count 12-hour waits from time of patients’ arrival in the Emergency Department to the time they are admitted to a ward. Measured in this way February and March 2022 show around one in five admissions through ED waited more than 12 hours from arriving until being admitted to a ward – equating to around 158,000 cases, 22% of attendances. Problems were particularly severe for people with mental health problems, with many examples of mental health patients waiting up to three days in emergency departments for a mental health inpatient bed to become available. When time was measured from time of arrival in the department to admission to a ward the figures of people waiting more than 12 hours were about six times greater than the nationally published figures which in July reached 29,317.
Wales
The Welsh NHS sets a measure of patients waiting more than 12 hours to be treated, transferred, and discharged by A&E. In January 2019, the Welsh NHS has recorded a record 6,882 patients waiting more than 12 hours in A&E, and Morriston Hospital in Swansea represented 15% of all A&E patients waiting more than 12 hours. The Welsh NHS Confederation responded to the figure by stating its disappointment but acknowledging numbers of patients attending with complex needs were increasing in Wales. Ambulance response times however improved and hit their target for the first time since October.Cancer
All across the UK the target is that patients should be treated within 62 days of an urgent referral, but the way this is measured varies. In Northern Ireland the target has not been met since 2015. The Welsh Government in 2019 became the first nation in the UK to have a single waiting times target for cancer treatment. In England 93% of patients referred for investigation of breast symptoms, even if cancer is not initially suspected, should be seen by a specialist within two weeks. Only 77.5% of patients referred for breast symptoms between April and June 2019 were seen within 2 weeks. Only 38% of hospitals met the target in 2019 and 22.5% of people waited longer than two months for their first treatment. In February 2022 10.7% of patients treated waited more than 104 days.Planned treatment
Over four million patients were waiting for non urgent hospital care as of July 2017. TheRoyal College of Surgeons
The Royal College of Surgeons is an ancient college (a form of corporation) established in England to regulate the activity of surgeons. Derivative organisations survive in many present and former members of the Commonwealth. These organisations a ...
together with other medical groups fear patients are waiting longer in anxiety and pain for hospital procedures. The target was that 90% of patients admitted to hospital for treatment and 95% of those not admitted should receive consultant-led care within 18 weeks unless it is clinically appropriate not to do so, or they choose to wait. The proportion of people waiting more than the six week target for diagnostic tests was at its highest since records began in September 2018. By August 2019 less than 49% of hospital services were achieving the target and across England the average wait was around 23 weeks. The clinical commissioning group
Clinical commissioning groups (CCGs) were NHS organisations set up by the Health and Social Care Act 2012 to organise the delivery of NHS services in each of their local areas in England. On 1 July 2022 they were abolished and replaced by Integra ...
joint committee for mid and south Essex in December 2019 reported that local hospitals were “now working” to a 40-week referral to treatment target.
One year wait
In December 2017 there were 1,750 patients waiting a year or more, the highest total since August 2012. 242 were atImperial College Healthcare NHS Trust
Imperial College Healthcare NHS Trust is an NHS trust based in London, England. It is one of the largest NHS trusts in England and together with Imperial College London forms an academic health science centre.
The trust was formed in October 20 ...
, 156 at Mid Essex Hospital Services NHS Trust
Mid Essex Hospital Services NHS Trust was an NHS trust which ran Broomfield Hospital in Chelmsford, St Peter's Hospital in Maldon, St Michael's Hospital in Braintree and formerly St John's Hospital in Chelmsford until its closure in 2010.
It ...
and 114 at Royal Cornwall Hospitals NHS Trust
The Royal Cornwall Hospitals NHS Trust is an NHS trust which runs West Cornwall Hospital, St Michael's Hospital, Royal Cornwall Hospital, and St Austell Hospital - Penrice Birthing Unit, in Cornwall, England.
History
The trust was established ...
. 11.8% of those waiting for a procedure had waited 18 weeks or more. By March 2018 there were 2,647. The largest numbers were at Northern Lincolnshire and Goole Hospitals NHS Foundation Trust
Northern Lincolnshire and Goole Hospitals NHS Foundation Trust is an NHS Foundation Trust which was established in April 2001, by a merger of North East Lincolnshire NHS Trust and Scunthorpe and Goole Hospitals NHS Trust. It runs the Diana, P ...
, Imperial College Healthcare NHS Trust
Imperial College Healthcare NHS Trust is an NHS trust based in London, England. It is one of the largest NHS trusts in England and together with Imperial College London forms an academic health science centre.
The trust was formed in October 20 ...
, King's College Hospital NHS Foundation Trust
King's College Hospital NHS Foundation Trust is an NHS trust in London, England. It is closely involved with Guy's and St Thomas' NHS Foundation Trust, with which it shares its chair, Sir Hugh Taylor, its strategy director and IT director. It ...
, Royal Cornwall Hospitals NHS Trust
The Royal Cornwall Hospitals NHS Trust is an NHS trust which runs West Cornwall Hospital, St Michael's Hospital, Royal Cornwall Hospital, and St Austell Hospital - Penrice Birthing Unit, in Cornwall, England.
History
The trust was established ...
and East Kent Hospitals University NHS Foundation Trust
East Kent Hospitals University NHS Foundation Trust is one of the largest hospital trusts in England. It runs the Kent and Canterbury Hospital (Canterbury), William Harvey Hospital (Ashford), Queen Elizabeth The Queen Mother Hospital (Margate), ...
. 2,432 patients had waited longer than a year in November 2018. In January 2019 NHS England announced that in future both providers and commissioners would be fined £2,500 for each such patient. In February 2022 299,478 patients had been on the list for over 52 weeks. Of those 23,281 had been waiting more than 2 years.
In Northern Ireland more than a third of patients, 94,222 people, had waited more than a year for their first appointment in October 2018. According to the Royal College of Surgeons in Ireland
The Royal College of Surgeons in Ireland (RCSI) is a medical professional and educational institution, which is also known as RCSI University of Medicine and Health Sciences, Ireland's first private university. It was established in 1784 ...
the 52-week target had "not been completely achieved in over 11 years".
In Wales a year target is not measured but a nine month target is monitored. As of January 2020 25,549 patients (5.5%) had been waiting more than nine months to receive treatment.
Six month wait
England
445,360 in England had been waiting six months or more by the end of December 2017 - three times more than in 2013. The President of theRoyal College of Surgeons
The Royal College of Surgeons is an ancient college (a form of corporation) established in England to regulate the activity of surgeons. Derivative organisations survive in many present and former members of the Commonwealth. These organisations a ...
said it was “completely shameful” that patients were being forced to resort to paying for operations the NHS should provide as these waiting times led to an increase of 53% between 2012 and 2016 in the numbers paying personally for private operations.
In July 2021 it was reported that there was a 46% increase in patients waiting more than 104 weeks for treatment, from 2,597 to 3,802 from April to May. There were 5.45 million people waiting for hospital treatment in England in JUne 2021 with very large differences in the numbers waiting in different areas, with 25 times more patients waiting for heart operations in Birmingham and Solihull than in West Lancashire.
Wales
In Wales, as of January 2020 83.5% of patients were waiting less than six months to start hospital treatment. This is the lowest figure since December 2015 and was below the Welsh Government's 95% target.Cancellations
Between January and March 2018 25,475 operations were cancelled at the last minute for non-clinical reasons by NHS providers - 20% more than the first quarter of 2017, and the highest number since records began in 1994–95. This was 1.3% of all elective activity - the highest proportion recorded since 2004–05.Community services
The 2019NHS Long Term Plan
The NHS Long Term Plan, also known as the NHS 10-Year Plan is a document published by NHS England on 7 January 2019, which sets out its priorities for healthcare over the next 10 years and shows how the NHS funding settlement will be used. It was p ...
proposed a two-hour standard for urgent community response services in England. These include prescribing and reviewing medication, access to physiotherapy and occupational therapy, and help with nutrition and hydration. Data has been collected since July 2020 and was first published in June 2022. The 70% two-hour response target was met at an all-England level but there were enormous variations between areas.
See also
* NHS ambulance services targetsReferences
{{reflist National Health Service (England) Emergency medical services in the United Kingdom NHS Scotland