|
Subutex
Buprenorphine is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection (intravenous and subcutaneous), as a skin patch (transdermal), or as an implant. For opioid use disorder, it is typically started when withdrawal symptoms have begun and for the first two days of treatment under direct observation of a health-care provider. In the United States, the combination formulation of buprenorphine/naloxone (Suboxone) is usually prescribed to discourage misuse by injection. Maximum pain relief is generally within an hour with effects up to 24 hours. Buprenorphine affects different types of opioid receptors in different ways. Depending on the type of receptor, it may be an agonist, partial agonist, or antagonist. In the treatment of opioid use disorder buprenorphine is an agonist/antagonist, meaning that it relieves withdrawal symptoms from other opioids and induces some euphori ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Sublingual
Sublingual (abbreviated SL), from the Latin for "under the tongue", refers to the pharmacological route of administration by which substances diffuse into the blood through tissues under the tongue. The sublingual glands receive their primary blood supply from the sublingual and submental arteries, which are branches of the lingual artery and facial artery, respectively. These arteries are both branches of the external carotid artery. The sublingual vein drains into the lingual vein, which then flows into the internal jugular system. The sublingual glands receive their parasympathetic input via the chorda tympani nerve, which is a branch of the facial nerve via the submandibular ganglion. The nerve functions in a secretomotor capacity. The chorda tympani branches from the motor branch of the facial nerve in the middle ear cavity, which then exits the middle ear through the petrotympanic fissure. The chorda tympani then travels with the lingual nerve to synapse at the subm ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Sublingual
Sublingual (abbreviated SL), from the Latin for "under the tongue", refers to the pharmacological route of administration by which substances diffuse into the blood through tissues under the tongue. The sublingual glands receive their primary blood supply from the sublingual and submental arteries, which are branches of the lingual artery and facial artery, respectively. These arteries are both branches of the external carotid artery. The sublingual vein drains into the lingual vein, which then flows into the internal jugular system. The sublingual glands receive their parasympathetic input via the chorda tympani nerve, which is a branch of the facial nerve via the submandibular ganglion. The nerve functions in a secretomotor capacity. The chorda tympani branches from the motor branch of the facial nerve in the middle ear cavity, which then exits the middle ear through the petrotympanic fissure. The chorda tympani then travels with the lingual nerve to synapse at the subm ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hypotension
Hypotension is low blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood. Blood pressure is indicated by two numbers, the systolic blood pressure (the top number) and the diastolic blood pressure (the bottom number), which are the maximum and minimum blood pressures, respectively. A systolic blood pressure of less than 90 millimeters of mercury (mmHg) or diastolic of less than 60 mmHg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present. Symptoms include dizziness or lightheadedness, confusion, feeling tired, weakness, headache, blurred vision, nausea, neck or back pain, an irregular heartbeat or feeling that the heart is skipping beats or fluttering, or fainting. Hypotension is the opposite of hypertension, which is high blood pressure. It is best understood as a physiological st ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
QT Prolongation
Long QT syndrome (LQTS) is a condition affecting repolarization (relaxing) of the heart after a heartbeat, giving rise to an abnormally lengthy QT interval. It results in an increased risk of an irregular heartbeat which can result in fainting, drowning, seizures, or sudden death. These episodes can be triggered by exercise or stress. Some rare forms of LQTS are associated with other symptoms and signs including deafness and periods of muscle weakness. Long QT syndrome may be present at birth or develop later in life. The inherited form may occur by itself or as part of larger genetic disorder. Onset later in life may result from certain medications, low blood potassium, low blood calcium, or heart failure. Medications that are implicated include certain antiarrhythmics, antibiotics, and antipsychotics. LQTS can be diagnosed using an electrocardiogram (EKG) if a corrected QT interval of greater than 480–500 milliseconds is found, but clinical findings, other EKG features, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
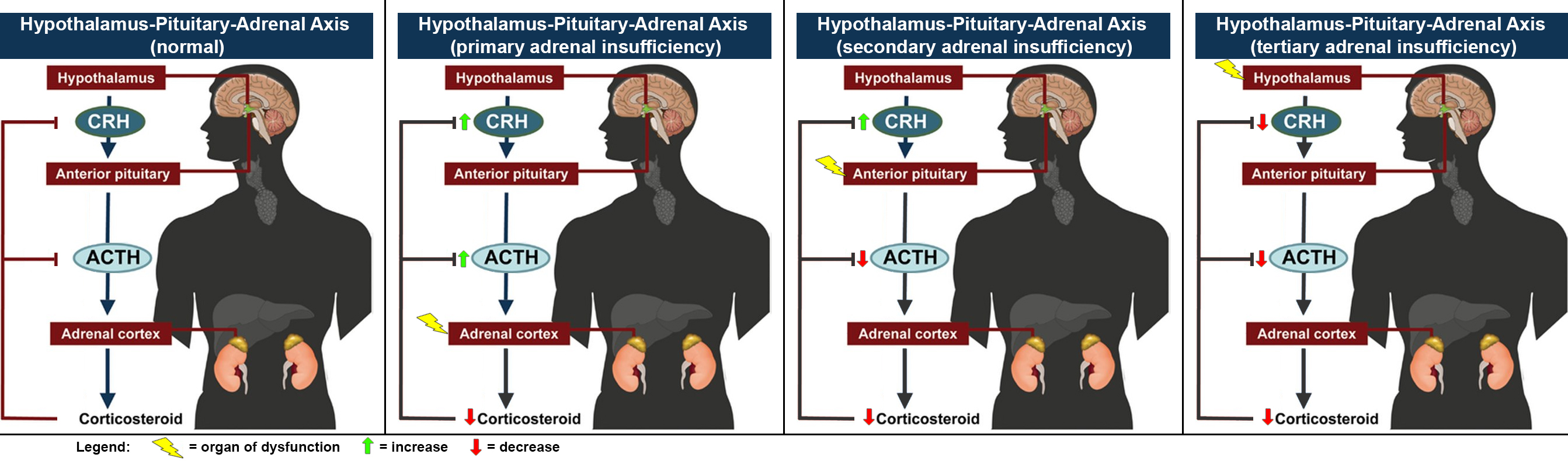
Adrenal Insufficiency
Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones. The adrenal gland normally secretes glucocorticoids (primarily cortisol), mineralocorticoids (primarily aldosterone), and androgens. These hormones are important in regulating blood pressure, electrolytes, and metabolism as a whole. Deficiency of these hormones leads to symptoms ranging from abdominal pain, vomiting, muscle weakness and fatigue, low blood pressure, depression, mood and personality changes (in mild cases) to organ failure and shock (in severe cases). An adrenal crisis may occur if the body is subjected to stress, such as an accident, injury, surgery, or severe infection; this is a life-threatening medical condition resulting from severe deficiency of cortisol in the body. Death may quickly follow. Adrenal insufficiency can be caused by dysfunction of the adrenal gland itself, whether by destruction (e.g. Addison's disease), failure of development ( ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Respiratory Depression
Hypoventilation (also known as respiratory depression) occurs when ventilation is inadequate (''hypo'' meaning "below") to perform needed respiratory gas exchange. By definition it causes an increased concentration of carbon dioxide (hypercapnia) and respiratory acidosis. Hypoventilation is not synonymous with respiratory arrest, in which breathing ceases entirely and death occurs within minutes due to hypoxia and leads rapidly into complete anoxia, although both are medical emergencies. Hypoventilation can be considered a precursor to hypoxia and its lethality is attributed to hypoxia with carbon dioxide toxicity. Causes Hypoventilation may be caused by: *A medical condition such as stroke affecting the brainstem *Voluntary breath-holding or underbreathing, for example, hypoventilation training or the Buteyko method. *Medication or drugs, typically when taken in accidental or intentional overdose. Opioids and benzodiazepines in particular are known to cause respiratory depress ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Receptor Antagonist
A receptor antagonist is a type of receptor ligand or drug that blocks or dampens a biological response by binding to and blocking a receptor rather than activating it like an agonist. Antagonist drugs interfere in the natural operation of receptor proteins.Pharmacology Guide: In vitro pharmacology: concentration-response curves " '' GlaxoWellcome.'' Retrieved on December 6, 2007. They are sometimes called blockers; examples include alpha blockers, |
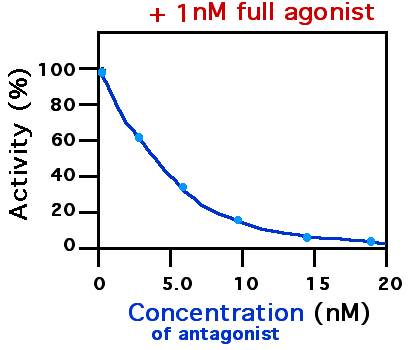
Partial Agonist
In pharmacology, partial agonists are drugs that bind to and activate a given receptor, but have only partial efficacy at the receptor relative to a full agonist. They may also be considered ligands which display both agonistic and antagonistic effects—when both a full agonist and partial agonist are present, the partial agonist actually acts as a competitive antagonist , competing with the full agonist for receptor occupancy and producing a net decrease in the receptor activation observed with the full agonist alone. Clinically, partial agonists can be used to activate receptors to give a desired submaximal response when inadequate amounts of the endogenous ligand are present, or they can reduce the overstimulation of receptors when excess amounts of the endogenous ligand are present. Some currently common drugs that have been classed as partial agonists at particular receptors include buspirone, aripiprazole, buprenorphine, nalmefene and norclozapine. Examples of ligands acti ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Agonist
An agonist is a chemical that activates a receptor to produce a biological response. Receptors are cellular proteins whose activation causes the cell to modify what it is currently doing. In contrast, an antagonist blocks the action of the agonist, while an inverse agonist causes an action opposite to that of the agonist. Etymology From the Greek αγωνιστής (agōnistēs), contestant; champion; rival < αγων (agōn), contest, combat; exertion, struggle < αγω (agō), I lead, lead towards, conduct; drive Types of agonists can be activated by either endogenous agonists (such as |
Opioid Receptors
Opioid receptors are a group of inhibitory G protein-coupled receptors with opioids as ligands. The endogenous opioids are dynorphins, enkephalins, endorphins, endomorphins and nociceptin. The opioid receptors are ~40% identical to somatostatin receptors (SSTRs). Opioid receptors are distributed widely in the brain, in the spinal cord, on peripheral neurons, and digestive tract. Discovery By the mid-1960s, it had become apparent from pharmacologic studies that opiate drugs were likely to exert their actions at specific receptor sites, and that there were likely to be multiple such sites. Early studies had indicated that opiates appeared to accumulate in the brain. The receptors were first identified as specific molecules through the use of binding studies, in which opiates that had been labeled with radioisotopes were found to bind to brain membrane homogenates. The first such study was published in 1971, using 3H-levorphanol. In 1973, Candace Pert and Solomon H. Snyder publis ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Buprenorphine/naloxone
Buprenorphine/naloxone, sold under the brand name Suboxone among others, is a fixed-dose combination medication that includes buprenorphine and naloxone. It is used to treat opioid use disorder, and reduces the mortality of opioid use disorder by 50% (by reducing the risk of overdose on full-agonist opioids such as heroin or fentanyl). It relieves cravings to use and withdrawal symptoms. Buprenorphine/naloxone is available for use in two different forms, under the tongue or in the cheek. Side effects may include respiratory depression (decreased breathing), small pupils, sleepiness, and low blood pressure. The risk of overdose with buprenorphine/naloxone (unless combined with other sedating substances) is exceedingly low, and lower than with methadone, but people are more likely to stop treatment on buprenorphine/naloxone than methadone. Buprenorphine (like methadone) is a treatment option during pregnancy. At lower doses, buprenorphine results in the usual opioid effects; ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Medical Implant
An implant is a medical device manufactured to replace a missing biological structure, support a damaged biological structure, or enhance an existing biological structure. Medical implants are man-made devices, in contrast to a transplant, which is a transplanted biomedical tissue. The surface of implants that contact the body might be made of a biomedical material such as titanium, silicone, or apatite depending on what is the most functional. In some cases implants contain electronics, e.g. artificial pacemaker and cochlear implants. Some implants are bioactive, such as subcutaneous drug delivery devices in the form of implantable pills or drug-eluting stents. Applications Implants can roughly be categorized into groups by application: Sensory and neurological Sensory and neurological implants are used for disorders affecting the major senses and the brain, as well as other neurological disorders. They are predominately used in the treatment of conditions such as catar ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |

.jpg)