|
Nomenclature Of Mechanical Ventilation
Many terms are used in mechanical ventilation, some are specific to brand, model, trademark and mode of mechanical ventilation. There is a standardized nomenclature of mechanical ventilation that is specific about nomenclature related to modes, but not settings and variables. Terms are now split into acronyms of CONTROL VARIABLE + BREATH SEQUENCE + TARGETING SCHEME. As in PC-CMV, Pressure Controlled Continuous Mandatory Ventilation. The term trigger (commonly flow or pressure) denotes the criteria that starts inspiration and cycle denotes the criteria that stops it. The target variable should not be confused with the cycle variable or the control variable. The target variable only sets an upper limit for pressure, volume or flow. Control variable The physical parameter that controls the breath in accordance with the equation of motion Equation of motion Pressure = Elastance*Volume + Resistance*Flow Volume control (VC) Volume controlled ventilation is ventilation where both vo ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Mechanical Ventilation
Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit. Mechanical ventilation is termed invasive if it involves an instrument to create an airway that is placed inside the trachea. This is done through an endotracheal tube or nasotracheal tube. For non-invasive ventilation in people who are conscious, face or nasal ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Minute Ventilation
Minute ventilation (or respiratory minute volume or minute volume) is the volume of gas inhaled (inhaled minute volume) or exhaled (exhaled minute volume) from a person's lungs per minute. It is an important parameter in respiratory medicine due to its relationship with blood carbon dioxide levels. It can be measured with devices such as a Wright respirometer or can be calculated from other known respiratory parameters. Although minute volume can be viewed as a unit of volume, it is usually treated in practice as a flow rate (given that it represents a volume change over time). Typical units involved are (in metric) 0.5 L × 12 breaths/min = 6 L/min. Several symbols can be used to represent minute volume. They include \dot (V̇ or V-dot) or Q (which are general symbols for flow rate), MV, and VE. Determination of minute volume Minute volume can either be measured directly or calculated from other known parameters. Measurement of minute volume Minute volume is the amo ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Respiratory Therapy
A respiratory therapist is a specialized healthcare practitioner trained in critical care and cardio-pulmonary medicine in order to work therapeutically with people who have acute critical conditions, cardiac and pulmonary disease. Respiratory therapists graduate from a college or university with a degree in respiratory therapy and have passed a national board certifying examination. The NBRC (National Board for Respiratory Care) is responsible for credentialing as a CRT ( certified respiratory therapist), or RRT ( registered respiratory therapist), The specialty certifications of respiratory therapy include: CPFT and RPFT (Certified or Registered Pulmonary Function Technologist), ACCS (Adult Critical Care Specialist), NPS (Neonatal/Pediatric Specialist), and SDS (Sleep Disorder Specialist). Respiratory therapists work in hospitals in the intensive care units (Adult, Pediatric, and Neonatal), on hospital floors, in emergency departments, in pulmonary functioning laboratories ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Expiratory Ratio
Exhalation (or expiration) is the flow of the breath out of an organism. In animals, it is the movement of air from the lungs out of the airways, to the external environment during breathing. This happens due to elastic properties of the lungs, as well as the internal intercostal muscles which lower the rib cage and decrease thoracic volume. As the thoracic diaphragm relaxes during exhalation it causes the tissue it has depressed to rise superiorly and put pressure on the lungs to expel the air. During forced exhalation, as when blowing out a candle, expiratory muscles including the abdominal muscles and internal intercostal muscles generate abdominal and thoracic pressure, which forces air out of the lungs. Exhaled air is 4% carbon dioxide, a waste product of cellular respiration during the production of energy, which is stored as ATP. Exhalation has a complementary relationship to inhalation which together make up the respiratory cycle of a breath. Exhalation and gas excha ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Positive End-expiratory Pressure
Positive end-expiratory pressure (PEEP) is the pressure in the lungs (alveolar pressure) above atmospheric pressure (the pressure outside of the body) that exists at the end of expiration. The two types of PEEP are extrinsic PEEP (PEEP applied by a ventilator) and intrinsic PEEP (PEEP caused by an incomplete exhalation). Pressure that is applied or increased during an inspiration is termed pressure support. Intrinsic (auto-) PEEP Auto-PEEP is an incomplete expiration prior to the initiation of the next breath causes progressive air trapping ( hyperinflation). This accumulation of air increases alveolar pressure at the end of expiration, which is referred to as auto-PEEP. Auto-PEEP develops commonly in high minute ventilation (hyperventilation), expiratory flow limitation (obstructed airway) and expiratory resistance (narrow airway). Once auto-PEEP is identified, steps should be taken to stop or reduce the pressure build-up. When auto-PEEP persists despite management of its ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Continuous Positive Airway Pressure
Continuous positive airway pressure (CPAP) is a form of positive airway pressure (PAP) ventilation in which a constant level of pressure greater than atmospheric pressure is continuously applied to the upper respiratory tract of a person. The application of positive pressure may be intended to prevent upper airway collapse, as occurs in obstructive sleep apnea, or to reduce the work of breathing in conditions such as acute decompensated heart failure. CPAP therapy is highly effective for managing obstructive sleep apnea. Compliance and acceptance of use of CPAP therapy can be a limiting factor, with 8% of people stopping use after the first night and 50% within the first year. Medical uses Severe to moderate obstructive sleep apnea CPAP is the most effective treatment for moderate to severe obstructive sleep apnea, in which the mild pressure from the CPAP prevents the airway from collapsing or becoming blocked. CPAP has been shown to be 100% effective at eliminating obs ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Mean Airway Pressure
Mean airway pressure typically refers to the mean pressure applied during positive-pressure mechanical ventilation. Mean airway pressure correlates with alveolar ventilation, arterial oxygenation, hemodynamic performance, and barotrauma. It can also match the alveolar pressure if there is no difference between inspiratory and expiratory resistance. Equations There are several equations aimed at determining the real mean airway pressure. Volume control ventilation In ventilation with a square flow waveform this equation can be used: \bar_=0.5\times(PIP - PEEP) \times (T_I/T_)+PEEP where: * \bar_ = mean airway pressure * PIP= peak inspiratory pressure * PEEP= peak end expiratory pressure * T_I= inspiratory time * T_= cycle time Pressure control ventilation During pressure control ventilation this variant of the equation can be used: \bar_= (PIP - PEEP) \times (T_I/T_)+PEEP where: * \bar_ = mean airway pressure * PIP= peak inspiratory pressure * PEEP= peak end expi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Plateau Pressure (airway)
Plateau pressure (PPLAT) is the pressure applied to small airways and alveoli during positive-pressure mechanical ventilation. It is measured during an inspiratory pause on the mechanical ventilator A ventilator is a piece of medical technology that provides mechanical ventilation by moving breathable air into and out of the lungs, to deliver breaths to a patient who is physically unable to breathe, or breathing insufficiently. Ventilators ....Moon, Richard and Enrico Camporesi “Respiratory Monitoring”. Miller’s Anesthesia, Sixth edition, Ronald Miller (Ed), 2005, Elsevier, New York. Pg.1466. In ARDS maintain plateau pressure <30cm of water measured on ventilator. References [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Peak Inspiratory Pressure
Peak inspiratory pressure (PIP) is the highest level of pressure applied to the lungs during inhalation. In mechanical ventilation Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move a ... the number reflects a positive pressure in centimeters of water pressure (cm H2O). In normal breathing, it may sometimes be referred to as the maximal inspiratory pressure (MIPO), which is a negative value. Peak inspiratory pressure increases with any airway resistance. Factors that may increase PIP include increased secretions, bronchospasm, biting down on ventilation tubing, and decreased lung compliance. PIP should never be chronically higher than 40 cm H2O unless the patient has acute respiratory distress syndrome. See also * Static compliance * Dynamic compliance References {{reflist Pulmonolog ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
High-frequency Ventilation
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. (>150 (Vf) breaths per minute) and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase. High-frequency ventilation may be used alone, or in combination with conventional mechanical ventilation. In general, those devices that need conventional mechanical ventilation do not produce the same lung protective effects as those that can operate without tidal breathing. Specifications and capabilities will vary depending on the device manufacturer. Physiology With conv ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Tidal Volume
Tidal volume (symbol VT or TV) is the volume of air moved into or out of the lungs during a normal breath. In a healthy, young human adult, tidal volume is approximately 500 ml per inspiration or 7 ml/kg of body mass. Mechanical ventilation Tidal volume plays a significant role during mechanical ventilation to ensure adequate ventilation without causing trauma to the lungs. Tidal volume is measured in milliliters and ventilation volumes are estimated based on a patient's ideal body mass. Measurement of tidal volume can be affected (usually overestimated) by leaks in the breathing circuit or the introduction of additional gas, for example during the introduction of nebulized drugs. Ventilator-induced lung injury such as Acute lung injury (ALI) /Acute Respiratory Distress Syndrome Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dy ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Mode Of Mechanical Ventilation
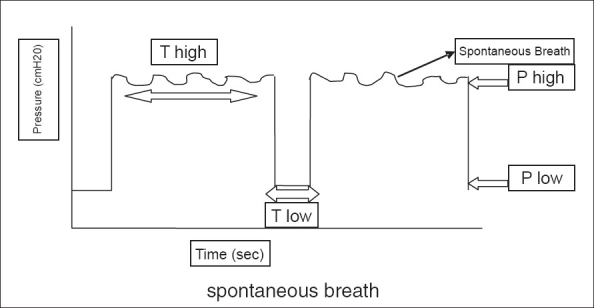
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy (i.e. PC-IMV, or VC-MMV etc.). Taxonomy for mechanical ventilation The taxonomy is a logical classification system based on 10 maxims of ventilator design 10 maxims #A breath is one cyc ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |