|
Ilioinguinal Nerve
The ilioinguinal nerve is a branch of the first lumbar nerve (L1). It separates from the first lumbar nerve along with the larger iliohypogastric nerve. It emerges from the lateral border of the psoas major just inferior to the iliohypogastric, and passes obliquely across the quadratus lumborum and iliacus. The ilioinguinal nerve then perforates the transversus abdominis near the anterior part of the iliac crest, and communicates with the iliohypogastric nerve between the transversus and the internal oblique muscle. It then pierces the internal oblique muscle, distributing filaments to it, and then accompanies the spermatic cord (in males) or the round ligament of uterus (in females) through the superficial inguinal ring. Its fibres are then distributed to the skin of the upper and medial part of the thigh, and to the following locations in the male and female: * In the male (" anterior scrotal nerve"): to the skin over the root of the penis and upper part of the scrotum. ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Lumbar Plexus
The lumbar plexus is a web of nerves (a nerve plexus) in the lumbar region of the body which forms part of the larger lumbosacral plexus. It is formed by the divisions of the first four lumbar nerves (L1–L4) and from contributions of the subcostal nerve (T12), which is the last thoracic nerve. Additionally, the ventral rami of the fourth lumbar nerve pass communicating branches, the lumbosacral trunk, to the sacral plexus. The nerves of the lumbar plexus pass in front of the hip joint and mainly support the anterior part of the thigh.''Thieme Atlas of anatomy'' (2006), pp 470-471 The plexus is formed lateral to the intervertebral foramina and passes through psoas major. Its smaller motor branches are distributed directly to psoas major, while the larger branches leave the muscle at various sites to run obliquely down through the pelvis to leave under the inguinal ligament with the exception of the obturator nerve which exits the pelvis through the obturator foramen. ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Round Ligament Of Uterus
The round ligament of the uterus is a ligament that connects the uterus to the labia majora. It originates at the junction of the uterus and uterine tube. It passes through the inguinal canal to insert at the labium majus. The two round ligaments of uterus develop from the gubernaculum; they are the female homologue of the male gubernaculum testis. Structure The round ligament of the uterus originates at the uterine horns, in the parametrium. The round ligament exits the pelvis via the deep inguinal ring. It passes through the inguinal canal to reach the labium majus, inserting into the fibro-fatty substance of the labium majus. Blood supply The round ligament is supplied by the artery of the round ligament of uterus, also known as ''Sampson's artery''. Development The round ligament develops from the gubernaculum which attaches the gonad to the labioscrotal swellings in the embryo. Function The round ligament of uterus acts to hold the uterus anterior-ward to in ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Caesarean Section
Caesarean section, also known as C-section, cesarean, or caesarean delivery, is the Surgery, surgical procedure by which one or more babies are Childbirth, delivered through an incision in the mother's abdomen. It is often performed because vaginal delivery would put the mother or child at risk (of paralysis or even death). Reasons for the operation include, but are not limited to, obstructed labor, twin pregnancy, pre-eclampsia, high blood pressure in the mother, breech birth, shoulder presentation, and problems with the placenta or umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's pelvis or history of a previous C-section. A trial of Vaginal birth after previous C-section, vaginal birth after C-section may be possible. The World Health Organization recommends that caesarean section be performed only when medically necessary. A C-section typically takes 45 minutes to an hour. It may be done with a spinal block, where the woman is awake ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hernia Repair
Hernia repair is a surgical operation for the correction of a hernia—a bulging of internal organs or tissues through the wall that contains it. It can be of two different types: herniorrhaphy; or hernioplasty. This operation may be performed to correct hernias of the abdomen, groin, diaphragm, brain, or at the site of a previous operation. Hernia repair is often performed as an ambulatory procedure. Techniques Inguinal hernia repair The first differentiating factor in hernia repair is whether the surgery is done open, or laparoscopically. Open hernia repair is when an incision is made in the skin directly over the hernia. Laparoscopic hernia repair is when minimally invasive cameras and equipment are used and the hernia is repaired with only small incisions adjacent to the hernia. These techniques are similar to the techniques used in laparoscopic gallbladder surgery. An operation in which the hernia sac is removed without any repair of the inguinal canal is described as ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Anesthesia
Anesthesia (American English) or anaesthesia (British English) is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia (relief from or prevention of pain), paralysis (muscle relaxation), amnesia (loss of memory), and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized. Anesthesia enables the painless performance of procedures that would otherwise require physical restraint in a non-anesthetized individual, or would otherwise be technically unfeasible. Three broad categories of anesthesia exist: * ''General anesthesia'' suppresses central nervous system activity and results in unconsciousness and total lack of Sensation (psychology), sensation, using either injected or inhaled drugs. * ''Sedation'' suppresses the central nervous system to a lesser degree, inhibiting both anxiolysis, anxiety and creation of long-term memory, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Nerve Block
Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. #Local anesthetic nerve block, Local anesthetic nerve block (sometimes referred to as simply "nerve block") is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed. The concept of nerve block sometimes includes ''central nerve block'', which includes epidural and spinal anaesthe ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Cremasteric Reflex
The cremasteric reflex is a superficial (i.e., close to the skin's surface) reflex observed in human males. This reflex is elicited by lightly stroking or poking the superior and medial (inner) part of the thigh—regardless of the direction of stroke. The normal response is an immediate contraction of the cremaster muscle that pulls up the testicle ipsilaterally (on the same side of the body). The reflex utilizes sensory and motor fibers from two different nerves. When the inner thigh is stroked, sensory fibers of the ilioinguinal nerve are stimulated. These activate the axon, motor fibers of the genital branch of the genitofemoral nerve which causes the cremaster muscle to contract and elevate the testis. Clinical conditions In some males this reflex may be exaggerated which can occasionally lead to a misdiagnosis of cryptorchidism. The cremasteric reflex may be absent with testicular torsion, upper and lower motor neuron disorders, as well as a spine injury of L1-L2. It can ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Inguinal Canal
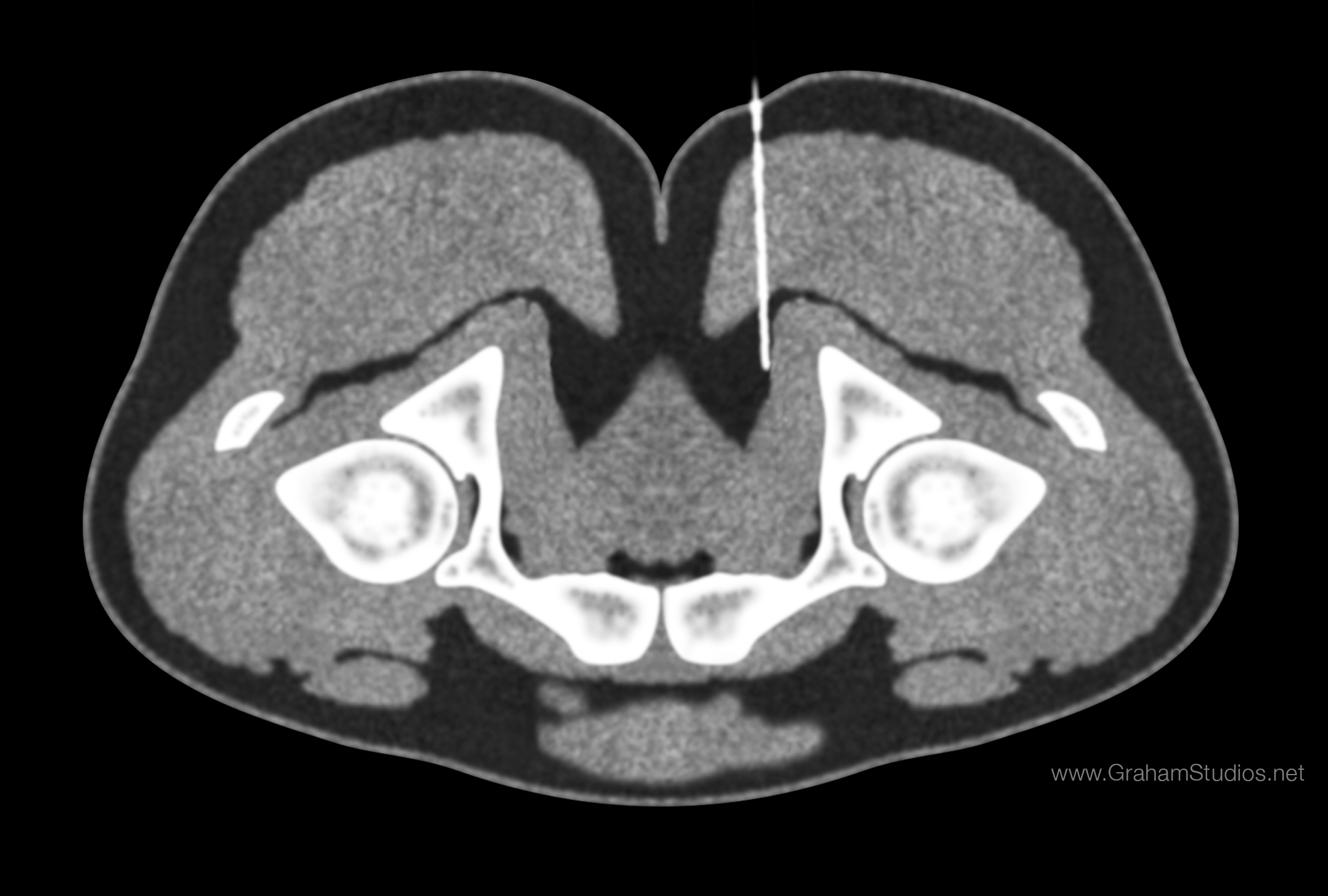
The inguinal canal is a passage in the anterior abdominal wall on each side of the body (one on each side of the midline), which in males, convey the spermatic cords and in females, the round ligament of the uterus. The inguinal canals are larger and more prominent in males. Structure The inguinal canals are situated just above the medial half of the inguinal ligament. The canals are approximately 4 to 6 cm long, angled anteroinferiorly and medially. In males, its diameter is normally 2 cm (±1 cm in standard deviation) at the deep inguinal ring.The diameter has been estimated to be ±2.2cm ±1.08cm in Africans, and 2.1 cm ±0.41cm in Europeans. A first-order approximation is to visualize each canal as a cylinder. Walls To help define the boundaries, these canals are often further approximated as boxes with six sides. Not including the two rings, the remaining four sides are usually called the "anterior wall", "inferior wall ("floor")", "superior wall ("roof")", and "po ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Deep Inguinal Ring
The inguinal canal is a passage in the anterior abdominal wall on each side of the body (one on each side of the midline), which in males, convey the spermatic cords and in females, the round ligament of the uterus. The inguinal canals are larger and more prominent in males. Structure The inguinal canals are situated just above the medial half of the inguinal ligament. The canals are approximately 4 to 6 cm long, angled anteroinferiorly and medially. In males, its diameter is normally 2 cm (±1 cm in standard deviation) at the deep inguinal ring.The diameter has been estimated to be ±2.2cm ±1.08cm in Africans, and 2.1 cm ±0.41cm in Europeans. A first-order approximation is to visualize each canal as a cylinder. Walls To help define the boundaries, these canals are often further approximated as boxes with six sides. Not including the two rings, the remaining four sides are usually called the "anterior wall", "inferior wall ("floor")", "superior wall ("roof")", and "poste ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Labia Majora
In primates, and specifically in humans, the labia majora (: labium majus), also known as the outer lips or outer labia, are two prominent Anatomical terms of location, longitudinal skin folds that extend downward and backward from the mons pubis to the perineum. Together with the labia minora, they form the labia of the vulva. The labia majora are Homology (biology), homologous to the male scrotum. Etymology ''Labia majora'' is the Latin plural for big ("major") lips. The Latin term ''labium/labia'' is used in anatomy for a number of usually paired parallel structures, but in English, it is mostly applied to two pairs of parts of the vulva—labia majora and labia minora. Traditionally, to avoid confusion with other lip-like structures of the body, the vulvar labia were termed by anatomists in Latin as ''labia majora (''or ''minora) pudendi.'' Embryology Embryologically, they develop from labioscrotal folds. The labia majora after puberty may become of a darker color than the ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Anterior Labial Nerve
The anterior labial nerves are branches of the ilioinguinal nerve. The nerves labia majora. The equivalent nerves in the male are the anterior scrotal nerves. See also * Posterior labial nerves The posterior labial nerves are superficial branches of the perineal nerve, which in itself is a branch of the pudendal nerve. The posterior labial nerves provide sensation to the labia majora and labia minora The labia minora (Latin for 'smalle ... References Nerves of the lower limb and lower torso {{neuroanatomy-stub ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Anterior Scrotal Nerve
The anterior scrotal nerves are branches of the ilioinguinal nerve. The nerves innervates the scrotum in males. The equivalent nerves in the female are the anterior labial nerves. See also * Posterior scrotal nerves The posterior scrotal branches are two in number, medial and lateral. They are branches of the perineal nerve, which is itself a branch of the pudendal nerve. The pudendal nerve arises from spinal roots S2 through S4, travels through the pudendal c ... Nerves of the lower limb and lower torso Scrotum {{neuroanatomy-stub ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |