|
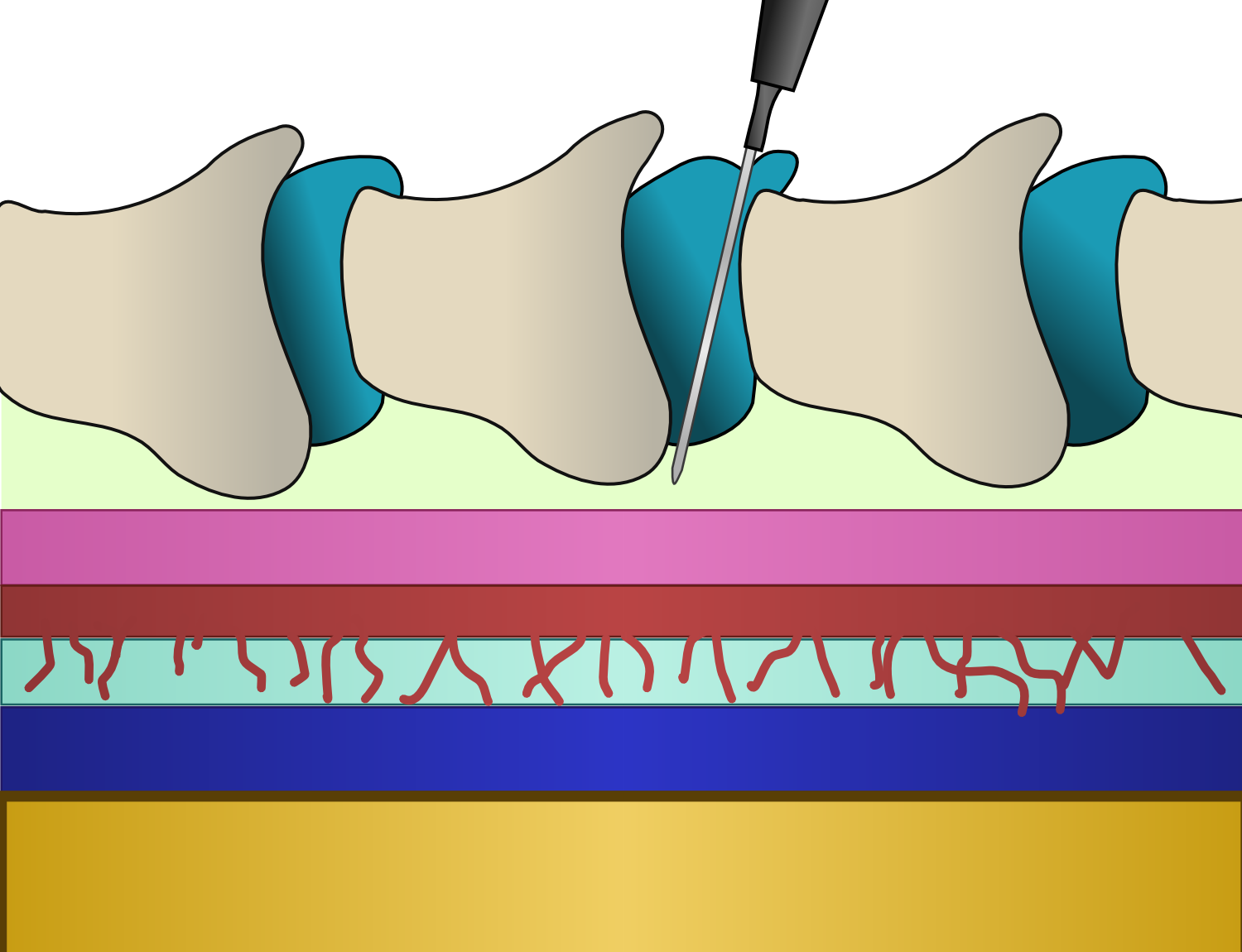
Epidural Lysis Of Adhesions
Epidural lysis of adhesions (LOA), also known as percutaneous adhesiolysis or the Racz procedure, is a minimally invasive spine surgery which involves the dissolution of epidural scar tissue by mechanical means to facilitate the spread of analgesics in an effort to alleviate pain. It is a type of percutaneous adhesiolysis procedure commonly used to treat chronic pain resulting from failed back surgery syndrome wherein scar tissue has formed around the nerves and causes pain. Evidence suggests the procedure may also be effective in treating spinal stenosis and radicular pain caused by a herniated disc. (Sometimes hyaluronidase (an enzyme) is also injected to dissolve the adhesions.) It was developed at Texas Tech University Health Sciences Center (TTUHSC) in 1989 by Gabor B. Racz. The procedure was assigned a Current Procedural Terminology (CPT) code in 2000. Etymology Epidural administration: injection into the epidural space of the spinal cord. Epidural, (Greek): situated on o ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Percutaneous
{{More citations needed, date=January 2021 In surgery, a percutaneous procedurei.e. Granger et al., 2012 is any medical procedure or method where access to inner organs or other tissue is done via needle-puncture of the skin, rather than by using an "open" approach where inner organs or tissue are exposed (typically with the use of a scalpel). The percutaneous approach is commonly used in vascular procedures such as angioplasty and stenting. This involves a needle catheter getting access to a blood vessel, followed by the introduction of a wire through the lumen (pathway) of the needle. It is over this wire that other catheters can be placed into the blood vessel. This technique is known as the modified Seldinger technique. More generally, "percutaneous", via its Latin roots means, 'by way of the skin'. An example would be percutaneous drug absorption from topical medications. More often, percutaneous is typically used in reference to placement of medical devices using a need ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Current Procedural Terminology
The Current Procedural Terminology (CPT) code set is a procedural code set developed by the American Medical Association (AMA). It is maintained by the CPT Editorial Panel. The CPT code set describes medical, surgical, and diagnostic services and is designed to communicate uniform information about medical services and procedures among physicians, coders, patients, accreditation organizations, and payers for administrative, financial, and analytical purposes. New editions are released each October, with CPT 2021 being in use since October 2021. It is available in both a standard edition and a professional edition. CPT coding is similar to ICD-10-CM coding, except that it identifies the services rendered, rather than the diagnosis on the claim. Whilst the ICD-10-PCS codes also contains procedure codes, those are only used in the inpatient setting. CPT is identified by the Centers for Medicare and Medicaid Services (CMS) as Level 1 of the Healthcare Common Procedure Coding Syste ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Epidural Anaesthesia
Epidural administration (from Ancient Greek ἐπί, , upon" + ''dura mater'') is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés. In the United States, over 50% of childbirths involve the use of epidural anesthesia. Epidural anaesthesia causes a loss of sensation, including pain, by blocking the transmission of signals through nerve fibres in or near the spinal cord. For this reason, epidurals are commonly used for pain cont ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Lysis
Lysis ( ) is the breaking down of the membrane of a cell, often by viral, enzymic, or osmotic (that is, "lytic" ) mechanisms that compromise its integrity. A fluid containing the contents of lysed cells is called a ''lysate''. In molecular biology, biochemistry, and cell biology laboratories, cell cultures may be subjected to lysis in the process of purifying their components, as in protein purification, DNA extraction, RNA extraction, or in purifying organelles. Many species of bacteria are subject to lysis by the enzyme lysozyme, found in animal saliva, egg white, and other secretions. Phage lytic enzymes (lysins) produced during bacteriophage infection are responsible for the ability of these viruses to lyse bacterial cells. Penicillin and related β-lactam antibiotics cause the death of bacteria through enzyme-mediated lysis that occurs after the drug causes the bacterium to form a defective cell wall. If the cell wall is completely lost and the penicillin was used ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Adhesion (medicine)
Adhesions are fibrous bands that form between tissues and organs, often as a result of injury during surgery. They may be thought of as internal scar tissue that connects tissues not normally connected. Pathophysiology Adhesions form as a natural part of the body's healing process after surgery in a similar way that a scar forms. The term "adhesion" is applied when the scar extends from within one tissue across to another, usually across a virtual space such as the peritoneal cavity. Adhesion formation post-surgery typically occurs when two injured surfaces are close to one another. According to the "classical paradigm" of adhesion formation, the pathogenesis starts with inflammation and activation of the coagulation system which causes fibrin deposits onto the damaged tissues. The fibrin then connects the two adjacent structures where damage of the tissues occurred. The fibrin acts like a glue to seal the injury and builds the fledgling adhesion, said at this point to be "fibrinou ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Dura Mater
In neuroanatomy, dura mater is a thick membrane made of dense irregular connective tissue that surrounds the brain and spinal cord. It is the outermost of the three layers of membrane called the meninges that protect the central nervous system. The other two meningeal layers are the arachnoid mater and the pia mater. It envelops the arachnoid mater, which is responsible for keeping in the cerebrospinal fluid. It is derived primarily from the neural crest cell population, with postnatal contributions of the paraxial mesoderm. Structure The dura mater has several functions and layers. The dura mater is a membrane that envelops the arachnoid mater. It surrounds and supports the dural sinuses (also called dural venous sinuses, cerebral sinuses, or cranial sinuses) and carries blood from the brain toward the heart. Cranial dura mater has two layers called ''lamellae'', a superficial layer (also called the periosteal layer), which serves as the skull's inner periosteum, called the ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Spinal Cord
The spinal cord is a long, thin, tubular structure made up of nervous tissue, which extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column (backbone). The backbone encloses the central canal of the spinal cord, which contains cerebrospinal fluid. The brain and spinal cord together make up the central nervous system (CNS). In humans, the spinal cord begins at the occipital bone, passing through the foramen magnum and then enters the spinal canal at the beginning of the cervical vertebrae. The spinal cord extends down to between the first and second lumbar vertebrae, where it ends. The enclosing bony vertebral column protects the relatively shorter spinal cord. It is around long in adult men and around long in adult women. The diameter of the spinal cord ranges from in the cervical and lumbar regions to in the thoracic area. The spinal cord functions primarily in the transmission of nerve signals from the motor cortex to the body, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Epidural Space
In anatomy, the epidural space is the potential space between the dura mater and vertebrae ( spine). The anatomy term "epidural space" has its origin in the Ancient Greek language; , "on, upon" + dura mater also known as "epidural cavity", "extradural space" or "peridural space". In humans the epidural space contains lymphatics, spinal nerve roots, loose connective tissue, adipose tissue, small arteries, dural venous sinuses and a network of internal vertebral venous plexuses. Cranial epidural space In the skull, the periosteal layer of the dura mater adheres to the inner surface of the skull bones while the meningeal layer lays over the arachnoid mater. Between them is the epidural space. The two layers of the dura mater separate at several places, with the meningeal layer projecting deeper into the brain parenchyma forming fibrous septa that compartmentalize the brain tissue. At these sites, the epidural space is wide enough to house the epidural venous sinuses. There are fo ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Epidural Administration
Epidural administration (from Ancient Greek ἐπί, , upon" + ''dura mater'') is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés. In the United States, over 50% of childbirths involve the use of epidural anesthesia. Epidural anaesthesia causes a loss of sensation, including pain, by blocking the transmission of signals through nerve fibres in or near the spinal cord. For this reason, epidurals are commonly used for pain cont ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
American Association Of Nurse Anesthetists
The American Association of Nurse Anesthesiology (AANA) is the professional association of nurse anesthetists in the United States. The organization states that it has a membership of more than 59,000, includes Certified Registered Nurse Anesthetist (CRNA) and student (SRNA) members. The organization represents approximately 90 percent of CRNAs in the United States. The AANA headquarters is currently located in Park Ridge, Illinois, a suburb of Chicago. The AANA held its first meeting on June 17, 1931. Agatha Hodgins organized the event, inviting members from the Alumnae Association of the Lakeside Hospital School of Anesthesia and other nurse anesthetists from across the United States. As a new organization, it had two main objectives: establish a national qualifying exam, and establish an accreditation program for nurse anesthesia schools. The first national certification exam was held on June 4, 1945, with 92 candidates sitting for the exam. The AANA has accredited nurse anes ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Minimally Invasive Spine Surgery
Minimally invasive spine surgery, also known as MISS, has no specific meaning or definition. It implies a lack of severe surgical invasion. The older style of open-spine surgery for a relatively small disc problem used to require a 5-6 inch incision and a month in the hospital. MISS techniques utilize more modern technology, advanced imaging techniques and special medical equipment to reduce tissue trauma, bleeding, radiation exposure, infection risk, and decreased hospital stays by minimizing the size of the incision. Modern endoscopic procedures (see below) can be done through a 2 to 5 mm skin opening. By contrast, procedures done with a microscope require skin openings of approximately one inch, or more. MISS can be used to treat a number of spinal conditions such as degenerative disc disease, disc herniation, fractures, tumors, infections, instability, and deformity. It also makes spine surgery possible for patients who were previously considered too high-risk for tradition ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |