|
Bronchopulmonary Dysplasia
Bronchopulmonary dysplasia (BPD; part of the spectrum of chronic lung disease of infancy) is a chronic lung disease in which premature infants, usually those who were treated with supplemental oxygen, require long-term oxygen. The alveoli that are present tend to not be mature enough to function normally. It is more common in infants with low birth weight (LBW) and those who receive prolonged mechanical ventilation to treat respiratory distress syndrome (RDS). It results in significant morbidity and mortality. The definition of BPD has continued to evolve primarily due to changes in the population, such as more survivors at earlier gestational ages, and improved neonatal management including surfactant, antenatal glucocorticoid therapy, and less aggressive mechanical ventilation. Currently the description of BPD includes the grading of its severity into mild, moderate and severe. This correlates with the infant's maturity, growth and overall severity of illness. The new system of ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
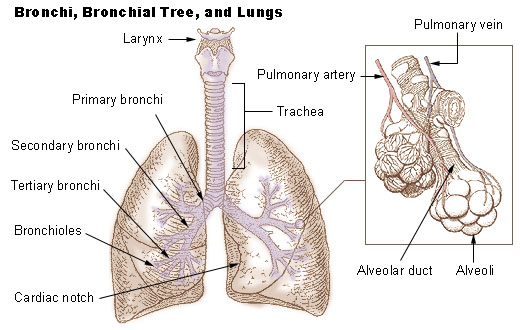
Lung
The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of the heart. Their function in the respiratory system is to extract oxygen from the air and transfer it into the bloodstream, and to release carbon dioxide from the bloodstream into the atmosphere, in a process of gas exchange. Respiration is driven by different muscular systems in different species. Mammals, reptiles and birds use their different muscles to support and foster breathing. In earlier tetrapods, air was driven into the lungs by the pharyngeal muscles via buccal pumping, a mechanism still seen in amphibians. In humans, the main muscle of respiration that drives breathing is the diaphragm. The lungs also provide airflow that makes vocal sounds including human speech possible. Humans have two lungs, one on the left and on ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Wilson–Mikity Syndrome
Wilson–Mikity syndrome, a form of chronic lung disease (CLD) that exists only in premature infants, leads to progressive or immediate development of respiratory distress. This rare condition affects low birth babies and is characterized by rapid development of lung emphysema after birth, requiring prolonged ventilation and oxygen supplementation. It is closely related to bronchopulmonary dysplasia (BPD), differing mainly in the lack of prior ventilatory support. All the initial patients described with Wilson–Mikity syndrome were very low birth weight infants that had no history of mechanical ventilation, yet developed a syndrome that clinically resembled BPD. Upon the death of some of these infants, autopsies showed histologic changes similar to those seen in BPD. It was characterized by Miriam G. Wilson and Victor G. Mikity in 1960. Symptoms and signs The onset of respiratory difficulty occurs at the first day of life and continues up to three weeks into the infant's life, ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
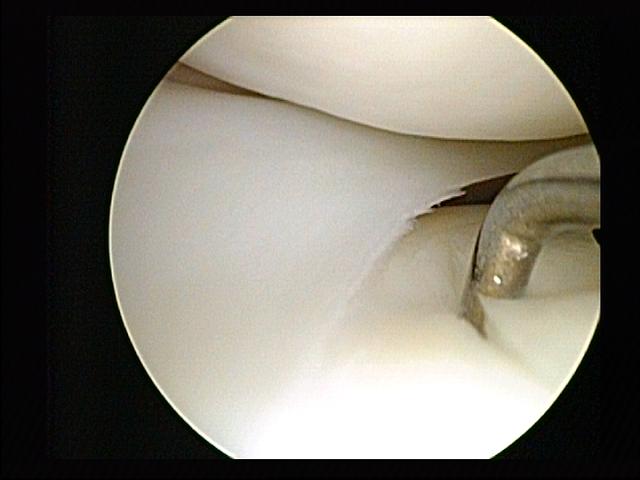
Minimally Invasive Procedure
Minimally invasive procedures (also known as minimally invasive surgeries) encompass surgical techniques that limit the size of incisions needed, thereby reducing wound healing time, associated pain, and risk of infection. Surgery by definition is invasive and many operations requiring incisions of some size are referred to as ''open surgery''. Incisions made during open surgery can sometimes leave large wounds that may be painful and take a long time to heal. Advancements in medical technologies have enabled the development and regular use of minimally invasive procedures. For example, endovascular aneurysm repair, a minimally invasive surgery, has become the most common method of repairing abdominal aortic aneurysms in the US as of 2003. The procedure involves much smaller incisions than the corresponding open surgery procedure of open aortic surgery. Interventional radiologists were the forerunners of minimally invasive procedures. Using imaging techniques, radiologists wer ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Exhalation
Exhalation (or expiration) is the flow of the breath out of an organism. In animals, it is the movement of air from the lungs out of the airways, to the external environment during breathing. This happens due to elastic properties of the lungs, as well as the internal intercostal muscles which lower the rib cage and decrease thoracic volume. As the thoracic diaphragm relaxes during exhalation it causes the tissue it has depressed to rise superiorly and put pressure on the lungs to expel the air. During forced exhalation, as when blowing out a candle, expiratory muscles including the abdominal muscles and internal intercostal muscles generate abdominal and thoracic pressure, which forces air out of the lungs. Exhaled air is 4% carbon dioxide, a waste product of cellular respiration during the production of energy, which is stored as ATP. Exhalation has a complementary relationship to inhalation which together make up the respiratory cycle of a breath. Exhalation and gas e ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Arterial Blood Gas Test
An arterial blood gas (ABG) test, or arterial blood gas analysis (ABGA) measures the amounts of arterial gases, such as oxygen and carbon dioxide. An ABG test requires that a small volume of blood be drawn from the radial artery with a syringe and a thin hypodermic needle, needle, but sometimes the femoral artery in the groin or another site is used. The blood can also be drawn from an arterial catheter. An ABG test measures the blood gas tension values of the Oxygen#Partial pressure, arterial partial pressure of oxygen (PaO2), and the PaCO2, arterial partial pressure of carbon dioxide (PaCO2), and the pH#Living systems, blood's pH. In addition, the arterial oxygen saturation (medicine), oxygen saturation (SaO2) can be determined. Such information is vital when caring for patients with critical illnesses or respiratory disease. Therefore, the ABG test is one of the most common tests performed on patients in intensive-care units. In other therapy#Levels of care, levels of care, pul ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hypocapnia
Hypocapnia (from the Greek words υπό meaning ''below normal'' and καπνός ''kapnós'' meaning ''smoke''), also known as hypocarbia, sometimes incorrectly called acapnia, is a state of reduced carbon dioxide in the blood. Hypocapnia usually results from deep or rapid breathing, known as hyperventilation. Hypocapnia is the opposite of hypercapnia. Effects Even when marked, hypocapnia is normally well tolerated. Symptoms include tingling sensation (usually in the limbs), abnormal heartbeat, painful muscle cramps, and seizures. Acute hypocapnia causes hypocapnic alkalosis, which causes cerebral vasoconstriction leading to cerebral hypoxia, and this can cause transient dizziness, fainting, and anxiety. A low partial pressure of carbon dioxide in the blood also causes alkalosis (because CO2 is acidic in solution), leading to lowered plasma calcium ions (Hypocalcaemia), causing increased nerve and muscle excitability. This explains the other common symptoms of hyperventilation&m ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hypercarbia
Hypercapnia (from the Greek ''hyper'' = "above" or "too much" and ''kapnos'' = "smoke"), also known as hypercarbia and CO2 retention, is a condition of abnormally elevated carbon dioxide (CO2) levels in the blood. Carbon dioxide is a gaseous product of the body's metabolism and is normally expelled through the lungs. Carbon dioxide may accumulate in any condition that causes hypoventilation, a reduction of alveolar ventilation (the clearance of air from the small sacs of the lung where gas exchange takes place) as well as resulting from inhalation of CO2. Inability of the lungs to clear carbon dioxide, or inhalation of elevated levels of CO2, leads to respiratory acidosis. Eventually the body compensates for the raised acidity by retaining alkali in the kidneys, a process known as "metabolic compensation". Acute hypercapnia is called acute hypercapnic respiratory failure (AHRF) and is a medical emergency as it generally occurs in the context of acute illness. Chronic hypercapn ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Oxygen Therapy
Oxygen therapy, also known as supplemental oxygen, is the use of oxygen as medical treatment. Acute indications for therapy include hypoxemia (low blood oxygen levels), carbon monoxide toxicity and cluster headache. It may also be prophylactically given to maintain blood oxygen levels during the induction of anesthesia. Oxygen therapy is often useful in chronic hypoxemia caused by conditions such as severe COPD or cystic fibrosis. Oxygen can be delivered via nasal cannula or face mask, or via high pressure conditions such as in endotracheal intubation or hyperbaric chamber. It can also be given through bypassing the airway, such as in ECMO therapy. Oxygen is required for normal cellular metabolism. However, excessively high concentrations can result in oxygen toxicity, leading to lung damage and respiratory failure. Higher oxygen concentrations can also increase the risk of airway fires, particularly while smoking. Oxygen therapy can also dry out the nasal mucosa without humidi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Acini
An acinus (; plural, acini; adjective, acinar or acinous) refers to any cluster of cells that resembles a many-lobed "berry," such as a raspberry ('' acinus'' is Latin for "berry"). The berry-shaped termination of an exocrine gland, where the secretion is produced, is acinar in form, as is the alveolar sac containing multiple alveoli in the lungs. Exocrine glands Acinar exocrine glands are found in many organs, including: * the stomach * the sebaceous gland of the scalp * the salivary glands of the tongue * the liver * the lacrimal glands * the mammary glands * the pancreas * the bulbourethral (Cowper's) glands The thyroid follicles can also be considered of acinar formation but in this case the follicles, being part of an ''endocrine'' gland, act as a hormonal deposit rather than to facilitate secretion. Mucous acini usually stain pale, while serous acini usually stain dark. Lungs The end of the terminal bronchioles in the lungs mark the beginning of a pulmonary acinus th ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
High Frequency Ventilation
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy (i.e. PC-IMV, or VC-MMV etc.). Taxonomy for mechanical ventilation The taxonomy is a logical classification system based on 10 maxims of ventilator design 10 maxims #A breath is one cy ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Surfactant Therapy
Surfactant therapy is the medical administration of exogenous surfactant. Surfactants used in this manner are typically instilled directly into the trachea. When a baby comes out of the womb and the lungs are not developed yet, they require administration of surfactant in order to process oxygen and survive. This condition that the baby has is called newborn respiratory distress syndrome, and it is treatable. Surfactant coat the smallest parts of the lungs called the alveoli and helps for oxygen to go in and for carbon dioxide to go out. How surfactant does this is by not allowing the alveoli to collapse and to retain their inflated shape when the baby exhales. In premature babies the type II pneumocytes, special lung cells that make surfactant, are not working yet. This means that the baby needs to get surfactant until that baby can make the surfactant on his own. In addition, the baby will need to be monitored and checked regularly as well as intubated or put on CPAP so that ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |