|
All-payer Rate Setting
All-payer rate setting is a price setting mechanism in which all third parties pay the same price for services at a given hospital. It can be used to increase the market power of payers (such as private and/or public insurance companies) versus providers, such as hospital systems, in order to control costs. All-payer characteristics are found in most developed economies with multi-payer healthcare systems, including France, Germany, Japan, and the Netherlands. The U.S. state of Maryland also uses such a model. All-payer rate setting have been proposed in the United States as a Healthcare reform in the United States, healthcare reform measure. The proposal for a public option (a voluntary, publicly sponsored insurance plan similar to Medicare (United States), Medicare) has been cited as indirectly sharing some of the same goals as all-payer rate-setting systems. Maryland Since the late 1970s, Maryland has operated an all-payer system for hospital services. An independent commissi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
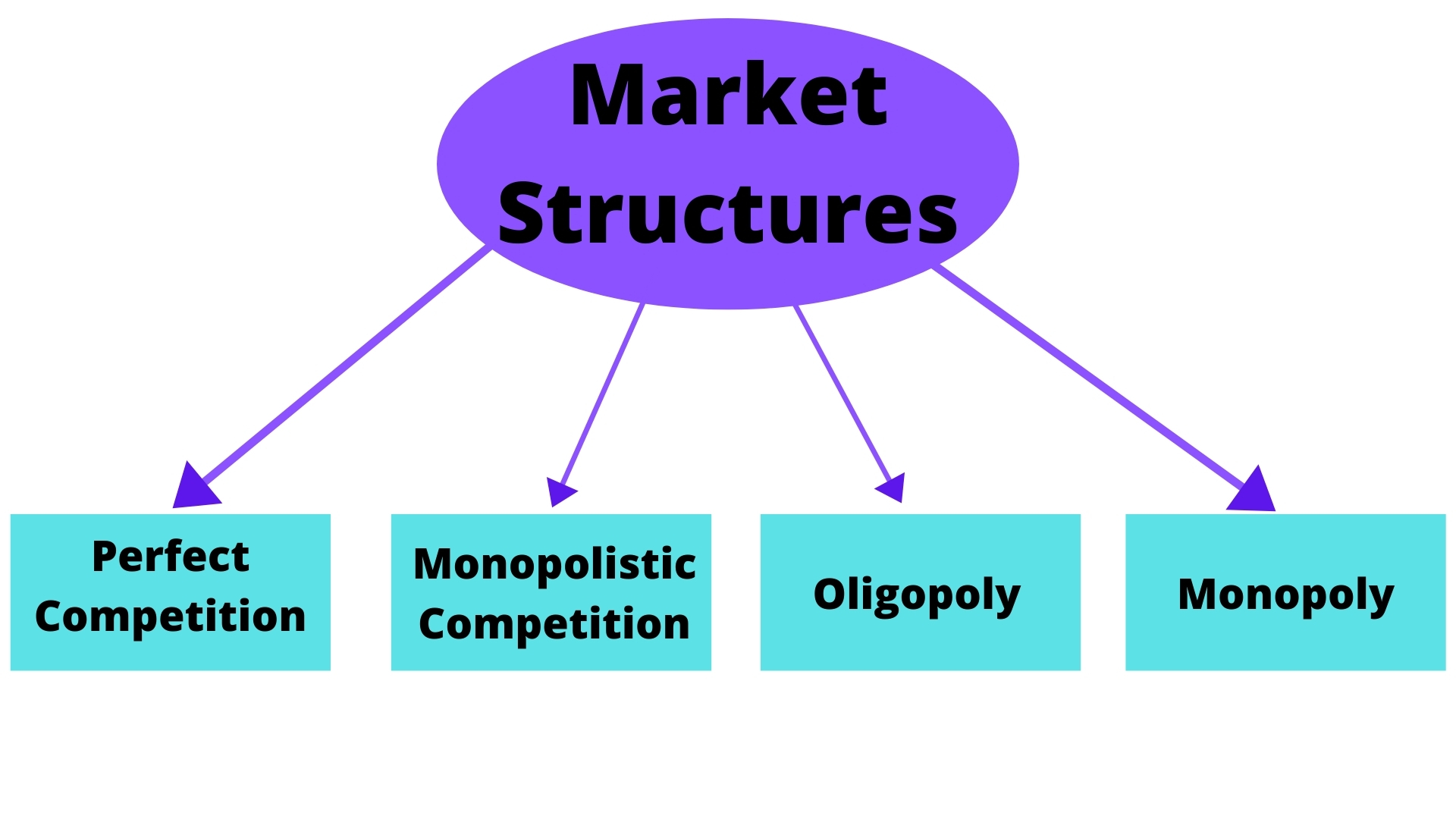
Market Power
In economics, market power refers to the ability of a firm to influence the price at which it sells a product or service by manipulating either the supply or demand of the product or service to increase economic profit. In other words, market power occurs if a firm does not face a perfectly elastic demand curve and can set its price (P) above marginal cost (MC) without losing revenue.Syverson, C. (2019). Macroeconomics and Market Power. The Journal of Economic Perspectives, 33(3), 23-43. https://doi.org/10.1257/jep.33.3.23 This indicates that the magnitude of market power is associated with the gap between P and MC at a firm's profit maximising level of output. Such propensities contradict perfectly competitive markets, where market participants have no market power, P = MC and firms earn zero economic profit. Market participants in perfectly competitive markets are consequently referred to as 'price takers', whereas market participants that exhibit market power are referred to as ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Medicare (United States)
Medicare is a government national health insurance program in the United States, begun in 1965 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, but also for some younger people with disability status as determined by the SSA, including people with end stage renal disease and amyotrophic lateral sclerosis (ALS or Lou Gehrig's disease). In 2018, according to the 2019 Medicare Trustees Report, Medicare provided health insurance for over 59.9 million individuals—more than 52 million people aged 65 and older and about 8 million younger people. According to annual Medicare Trustees reports and research by the government's MedPAC group, Medicare covers about half of healthcare expenses of those enrolled. Enrollees almost always cover most of the remaining costs by taking additional private insurance and/or by joining a public Part C or P ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Single-payer Health Care
Single-payer healthcare is a type of universal healthcare in which the costs of essential healthcare for all residents are covered by a single public system (hence "single-payer"). Single-payer systems may contract for healthcare services from private organizations (as is the case in Canada) or may own and employ healthcare resources and personnel (as is the case in the United Kingdom). "Single-payer" describes the mechanism by which healthcare is paid for by a single public authority, not a private authority, nor a mix of both. Description Within single-payer healthcare systems, a single government or government-related source pays for all covered healthcare services.Medical Subject Headings thesaurus, National Library of Medicin"Single-Payer System" Year introduced: 1996, (From Slee and Slee, Health Care Reform Terms, 1993, p. 106) Governments use this strategy to achieve several goals, including universal healthcare, decreased economic burden of health care, and improved heal ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Fee-for-service
Fee-for-service (FFS) is a payment model where services are unbundled and paid for separately. In health care, it gives an incentive for physicians to provide more treatments because payment is dependent on the quantity of care, rather than quality of care. However evidence of the effectiveness of FFS in improving health care quality is mixed, without conclusive proof that these programs either succeed or fail. Similarly, when patients are shielded from paying (cost-sharing) by health insurance coverage, they are incentivized to welcome any medical service that might do some good. Fee-for-services raises costs, and discourages the efficiencies of integrated care. A variety of reform efforts have been attempted, recommended, or initiated to reduce its influence (such as moving towards bundled payments and capitation). In capitation, physicians are not incentivized to perform procedures, including necessary ones, because they are not paid anything extra for performing them. FFS is t ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Capitation (healthcare)
Capitation is a payment arrangement for health care service providers. It pays a set amount for each enrolled person assigned to them, per period of time, whether or not that person seeks care. The amount of remuneration is based on the average expected health care utilization of that patient, with payment for patients generally varying by age and health status. Types There are differing arrangements in different healthcare systems. Capitation in the USA Primary capitation is a relationship between a managed care organization and primary care physician, in which the physician is paid directly by the organization for those who have selected the physician as their provider. Secondary capitation is a relationship arranged by a managed care organization between a physician and a secondary or specialist provider, such as an X-ray facility or ancillary facility such as a durable medical equipment supplier whose secondary provider is also paid capitation based on that PCP's enrolled ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Centers For Medicare And Medicaid Services
The Centers for Medicare & Medicaid Services (CMS), is a federal agency within the United States Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid, the Children's Health Insurance Program (CHIP), and health insurance portability standards. In addition to these programs, CMS has other responsibilities, including the administrative simplification standards from the Health Insurance Portability and Accountability Act of 1996 (HIPAA), quality standards in long-term care facilities (more commonly referred to as nursing homes) through its survey and certification process, clinical laboratory quality standards under the Clinical Laboratory Improvement Amendments, and oversight of HealthCare.gov. CMS was previously known as the Health Care Financing Administration (HCFA) until 2001. CMS actively inspects and reports on every nursing home in the United States. This includes maintaini ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Prospective Payment System
A prospective payment system (PPS) is a term used to refer to several payment methodologies for which means of determining insurance reimbursement is based on a predetermined payment regardless of the intensity of the actual service provided. It includes a system for paying hospitals based on predetermined prices, from Medicare. Payments are typically based on codes provided on the insurance claim such as these: * Diagnosis-related groups for hospital inpatient claims * Ambulatory Payment Classification for hospital outpatient claims * Current Procedural Terminology for other outpatient claims The PPS was established by the Centers for Medicare and Medicaid Services (CMS), as a result of the Social Security Amendments Act of 1983, specifically to address expensive hospital care. Regardless of services provided, payment was of an established fee. The idea was to encourage hospitals to lower their prices for expensive hospital care. In 2000, CMS changed the reimbursement system ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Social Security Act
The Social Security Act of 1935 is a law enacted by the 74th United States Congress and signed into law by US President Franklin D. Roosevelt. The law created the Social Security program as well as insurance against unemployment. The law was part of Roosevelt's New Deal domestic program. By the 1930s, the United States was the only modern industrial country without any national system of social security. In the midst of the Great Depression, the physician Francis Townsend galvanized support behind a proposal to issue direct payments to the elderly. Responding to that movement, Roosevelt organized a committee led by Secretary of Labor Frances Perkins to develop a major social welfare program proposal. Roosevelt presented the plan in early 1935 and signed the Social Security Act into law on August 14, 1935. The act was upheld by the Supreme Court in two major cases decided in 1937. The law established the Social Security program. The old-age program is funded by payroll taxes, an ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Per Capita
''Per capita'' is a Latin phrase literally meaning "by heads" or "for each head", and idiomatically used to mean "per person". The term is used in a wide variety of social sciences and statistical research contexts, including government statistics, economic indicators, and built environment studies. It is commonly used in the field of statistics in place of saying "per person" (although ''per caput'' is the Latin for "per head"). It is also used in wills to indicate that each of the named beneficiaries should receive, by devise or bequest, equal shares of the estate. This is in contrast to a ''per stirpes'' division, in which each branch (Latin ''stirps'', plural ''stirpes'') of the inheriting family inherits an equal share of the estate. This is often used with the ‘2-0 rule’, a statistical principle that determines which group is larger per capita. Under the 2-0 rule, a group is the largest per capita if it has both the biggest total size and size of the group of the obje ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Public Option
The public health insurance option, also known as the public insurance option or the public option, is a proposal to create a government-run health insurance agency that would compete with other private health insurance companies within the United States. The public option is not the same as publicly funded health care, but was proposed as an alternative health insurance plan offered by the government. The public option was initially proposed for the Patient Protection and Affordable Care Act, but was removed after independent Connecticut senator Joe Lieberman threatened a filibuster.Lieberman: I'll block vote on Reid plan By Manu Raju, Politico.com, 10/27/09 Subsequently, Congress did not include the public option in the bill passed under reconciliatio ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hospital System
A hospital network is a public, non-profit or for-profit company or organization that provides two or more hospitals and other broad healthcare facilities and services. A hospital network may include hospitals in one or more regions within one or more states within one or more countries. A hospital network has one headquarter, usually within one of the regions served by the network facilities. (The term hospital system or health care system is used more broadly to define the organization of people, institutions, and resources that deliver health care services to meet the health needs of a region or country.) History Some of the earliest hospital networks were affiliated with charitable, religious organizations. The Catholic Church established a hospital network in Medieval Europe that was vastly improved from the merely reciprocal hospitality of the Greeks and family-based obligations of the Romans. These hospitals were established to cater to "particular social groups margi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Healthcare Reform In The United States
Healthcare reform in the United States has a long history. Reforms have often been proposed but have rarely been accomplished. In 2010, landmark reform was passed through two federal statutes enacted in 2010: the Patient Protection and Affordable Care Act (PPACA), signed March 23, 2010, and the Health Care and Education Reconciliation Act of 2010 (), which amended the PPACA and became law on March 30, 2010. Future reforms of the American health care system continue to be proposed, with notable proposals including a single-payer system and a reduction in fee-for-service medical care. The PPACA includes a new agency, the Center for Medicare and Medicaid Innovation (CMS Innovation Center), which is intended to research reform ideas through pilot projects. History of national reform efforts The following is a summary of reform achievements at the national level in the United States. For failed efforts, state-based efforts, native tribes services, and more details, see the histor ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |