|
Pharmacy Benefit Manager
In the United States, a pharmacy benefit manager (PBM) is a third-party administrator of prescription drug programs for commercial health plans, self-insured employer plans, Medicare Part D plans, the Federal Employees Health Benefits Program, and state government employee plans. According to the American Pharmacists Association, "PBMs are primarily responsible for developing and maintaining the formulary, contracting with pharmacies, negotiating discounts and rebates with drug manufacturers, and processing and paying prescription drug claims." PBMs operate inside of integrated healthcare systems (e.g., Kaiser Permanente or Veterans Health Administration), as part of retail pharmacies (e.g., CVS Pharmacy or Rite-Aid), and as part of insurance companies (e.g., UnitedHealth Group). As of 2016, PBMs managed pharmacy benefits for 266 million Americans. In 2017, the largest PBMs had higher revenue than the largest pharmaceutical manufacturers, indicating their increasingly large r ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Third-party Administrator
In the United States, a third-party administrator (TPA) is an organization that processes insurance claims or certain aspects of employee benefit plans for a separate entity. It is also a term used to define organizations within the insurance industry which administer other services such as underwriting and customer service. This can be viewed as outsourcing the administration of the claims processing, since the TPA is performing a task traditionally handled by the company providing the insurance or the company itself. Often, in the case of insurance claims, a TPA handles the claims processing for an employer that self-insures its employees. Thus, the employer is acting as an insurance company and underwrites the risk. The risk of loss remains with the employer, and not with the TPA. An insurance company may also use a TPA to manage its claims processing, provider networks, utilization review, or membership functions. While some third-party administrators may operate as units of ins ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Collective Buying Power
Collective buying power is the ability of a group of consumers to leverage the group size in exchange for discounts. In the marketplace Many different companies have used this concept to build business plans. Warehouse clubs function in a similar way by offering products in bulk to consumers who pay membership fees. In the same sense collective buying power is a cooperative approach to leveraging group size to benefit the consumer by offering Internet companies have been leveraging this concept, bringing people together online. The company will arrange a coupon offering, that will only go into effect if more than a before agreed upon number are sold. Dental industry example One example of a business plan that uses collective buying power is found in the dental industry. Discount dental plans negotiate discounts for dental services on behalf of their members. Depending on the details, it may sometimes be considered a win-win scenario for the discount plan members (dental pat ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Generic Drug
A generic drug is a pharmaceutical drug that contains the same chemical substance as a drug that was originally protected by chemical patents. Generic drugs are allowed for sale after the patents on the original drugs expire. Because the active chemical substance is the same, the medical profile of generics is equivalent in performance. A generic drug has the same active pharmaceutical ingredient (API) as the original, but it may differ in some characteristics such as the manufacturing process, formulation, excipients, color, taste, and packaging. Although they may not be associated with a particular company, generic drugs are usually subject to government regulations in the countries in which they are dispensed. They are labeled with the name of the manufacturer and a generic non-proprietary name such as the United States Adopted Name (USAN) or International Nonproprietary Name (INN) of the drug. A generic drug must contain the same active ingredients as the original brand-name ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Managed Care
The term managed care or managed healthcare is used in the United States to describe a group of activities intended to reduce the cost of providing health care and providing American health insurance while improving the quality of that care ("managed care techniques"). It has become the predominant system of delivering and receiving American health care since its implementation in the early 1980s, and has been largely unaffected by the Affordable Care Act of 2010. ...intended to reduce unnecessary health care costs through a variety of mechanisms, including: economic incentives for physicians and patients to select less costly forms of care; programs for reviewing the medical necessity of specific services; increased beneficiary cost sharing; controls on inpatient admissions and lengths of stay; the establishment of cost-sharing incentives for outpatient surgery; selective contracting with health care providers; and the intensive management of high-cost health care cases. The p ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Healthcare Service
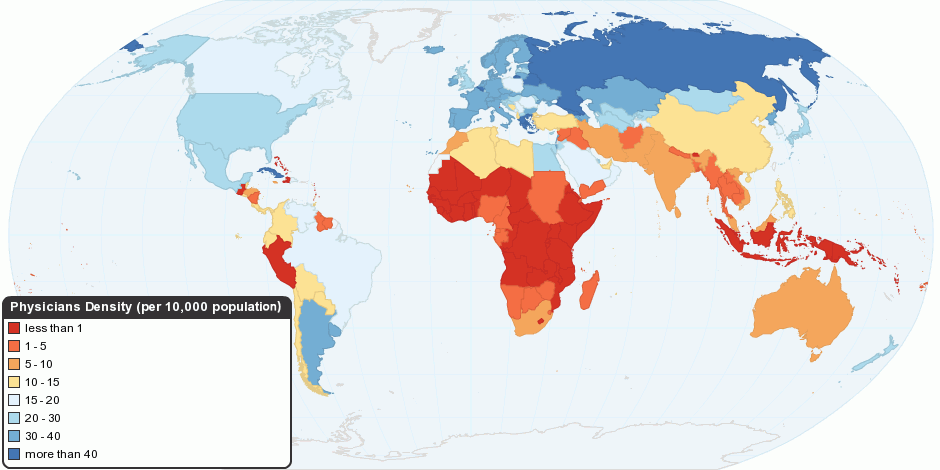
Health care or healthcare is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. It includes work done in providing primary care, secondary care, and tertiary care, as well as in public health. Access to health care may vary across countries, communities, and individuals, influenced by social and economic conditions as well as health policies. Providing health care services means "the timely use of personal health services to achieve the best possible health outcomes". Factors to consider in terms of health care access include financial limitations (such as insurance coverage), geographi ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
SmithKline Beecham
GSK plc, formerly GlaxoSmithKline plc, is a British multinational pharmaceutical and biotechnology company with global headquarters in London, England. Established in 2000 by a merger of Glaxo Wellcome and SmithKline Beecham. GSK is the tenth largest pharmaceutical company and #294 on the 2022 ''Fortune'' Global 500, ranked behind other pharmaceutical companies China Resources, Sinopharm, Johnson & Johnson, Pfizer, Roche, AbbVie, Novartis, Bayer, and Merck. The company has a primary listing on the London Stock Exchange and is a constituent of the FTSE 100 Index. , it had a market capitalisation of £70 billion, the eighth largest on the London Stock Exchange. It has a secondary listing on the New York Stock Exchange. The company developed the first malaria vaccine, RTS,S, which it said in 2014 it would make available for five percent above cost. Legacy products developed at GSK include several listed in the World Health Organization's List of Essential Medicines, such ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
United HealthGroup
UnitedHealth Group Incorporated is an American multinational managed healthcare and insurance company based in Minnetonka, Minnesota. It offers health care products and insurance services. UnitedHealth Group is the world's seventh largest company by revenue and the largest healthcare company by revenue, and the largest insurance company by net premiums. UnitedHealthcare revenues comprise 80% of the Group's overall revenue. The company is ranked 11th on the 2022 Fortune Global 500. UnitedHealth Group has a market capitalization of $400.7 billion as of March 31, 2021. History In 1974, Richard Taylor Burke founded Charter Med Incorporated, a Minnetonka, Minnesota-based privately held company. In 1977, the United HealthCare Corporation was created to reorganize the company and became the parent company of Charter Med. United HealthCare's charter was to manage the newly created Physicians Health Plan of Minnesota, an early health management organization. In 1988, United HealthC ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Health Maintenance Organization
In the United States, a health maintenance organization (HMO) is a medical insurance group that provides health services for a fixed annual fee. It is an organization that provides or arranges managed care for health insurance, self-funded health care benefit plans, individuals, and other entities, acting as a liaison with health care providers (hospitals, doctors, etc.) on a prepaid basis. The Health Maintenance Organization Act of 1973 required employers with 25 or more employees to offer federally certified HMO options if the employer offers traditional healthcare options. Unlike traditional indemnity insurance, an HMO covers care rendered by those doctors and other professionals who have agreed by contract to treat patients in accordance with the HMO's guidelines and restrictions in exchange for a steady stream of customers. HMOs cover emergency care regardless of the health care provider's contracted status. Operation HMOs often require members to select a primary care phy ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Diversified Pharmaceutical Services
Diversified Pharmaceutical Services entered the market in 1976 as the pharmacy benefit manager for United HealthCare, a leading managed care organization. It pioneered many cost containment strategies that are now core pharmacy benefit manager services and became a recognized leader in clinical programs. History Diversified Pharmaceutical Services (DPS) grew out of the pharmacy department within United Healthcare. The company was sold to SmithKline Beecham GSK plc, formerly GlaxoSmithKline plc, is a British multinational pharmaceutical and biotechnology company with global headquarters in London, England. Established in 2000 by a merger of Glaxo Wellcome and SmithKline Beecham. GSK is the tent ... for $2.3 billion in May 1994. In 1999, it was acquired by Express Scripts in 1999 for $700 million in cash to create what was then the third largest pharmacy benefit manager in the United States. References Health maintenance organizations Life sciences industry Medica ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
AdvancePCS
AdvancePCS Inc. (Pharmaceutical Card System) was a large prescription benefit plan administrator from the United States, also known as a PBM (Pharmacy Benefit Manager). The company was partially purchased by McKesson in 1969 and fully in 1972. In 1994, the company was sold to Lilly for $4.4 billion. Rite Aid Rite Aid Corporation is an American drugstore chain based in Philadelphia, Pennsylvania. It was founded in 1962 in Scranton, Pennsylvania, by Alex Grass under the name Thrift D Discount Center. The company ranked No. 148 in the Fortune 500 lis ... purchased AdvancePCS for $1.5 billion in 1999, but sold to Advance Paradigm a year later for $1 billion. In 2003, Caremark bought AdvancePCS for $5.3 billion, and CVS acquired Caremark in 2007 in a $26.5 billion deal. [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Caremark Rx
CVS Caremark (formerly Caremark Rx) (stylized as , previously CVS/caremark) is the prescription benefit management subsidiary of CVS Health, headquartered in Woonsocket, Rhode Island. Company history Caremark was founded as a physician and pharmacy benefits management company in 1993. It was founded in Birmingham, Alabama as MedPartners, Inc. by former HealthSouth Corporation chief executive Richard Scrushy. New Enterprise Associates was an initial investor in the company. MedPartners went public in February of 1995. In August 1995, MedPartners announced the acquisition of Mullikin Medical Enterprises, a physician management company. In December 1995, MedPartners acquired Pacific Physicians Services in Redlands, California. On May 15, 1996, Caremark International, a provider of manager health services, announced it would be acquired by MedPartners. Caremark International was founded as a unit of Baxter International and was spun off from Baxter in 1992 as a publicly traded c ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Copayment
A copayment or copay (called a gap in Australian English) is a fixed amount for a covered service, paid by a patient to the provider of service before receiving the service. It may be defined in an insurance policy and paid by an insured person each time a medical service is accessed. It is technically a form of coinsurance, but is defined differently in health insurance where a coinsurance is a percentage payment after the deductible up to a certain limit. It must be paid before any policy benefit is payable by an insurance company. Copayments do not usually contribute towards any policy out-of-pocket maximum, whereas coinsurance payments do. Insurance companies use copayments to share health care costs to prevent moral hazard. It may be a small portion of the actual cost of the medical service but is meant to deter people from seeking medical care that may not be necessary, e.g., an infection by the common cold. In health systems with prices below the market clearing level in wh ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |