|
Glycogen Storage Disease
A glycogen storage disease (GSD, also glycogenosis and dextrinosis) is a metabolic disorder caused by an enzyme deficiency affecting glycogen synthesis, glycogen breakdown, or glucose breakdown, typically in muscles and/or liver cells. GSD has two classes of cause: genetic and acquired. Genetic GSD is caused by any inborn error of metabolism (genetically defective enzymes) involved in these processes. In livestock, acquired GSD is caused by intoxication with the alkaloid castanospermine. Types Remarks: * Some GSDs have different forms, e.g. infantile, juvenile, adult (late-onset). * Some GSDs have different subtypes, e.g. GSD1a / GSD1b, GSD9A1 / GSD9A2 / GSD9B / GSD9C / GSD9D. * GSD type 0: Although glycogen synthase deficiency does not result in storage of extra glycogen in the liver, it is often classified with the GSDs as type 0 because it is another defect of glycogen storage and can cause similar problems. * GSD type VIII (GSD 8): In the past it was considered a distin ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Glycogen
Glycogen is a multibranched polysaccharide of glucose that serves as a form of energy storage in animals, fungi, and bacteria. The polysaccharide structure represents the main storage form of glucose in the body. Glycogen functions as one of two forms of energy reserves, glycogen being for short-term and the other form being triglyceride stores in adipose tissue (i.e., body fat) for long-term storage. In humans, glycogen is made and stored primarily in the cells of the liver and skeletal muscle. In the liver, glycogen can make up 5–6% of the organ's fresh weight, and the liver of an adult, weighing 1.5 kg, can store roughly 100–120 grams of glycogen. In skeletal muscle, glycogen is found in a low concentration (1–2% of the muscle mass) and the skeletal muscle of an adult weighing 70 kg stores roughly 400 grams of glycogen. The amount of glycogen stored in the body—particularly within the muscles and liver—mostly depends on physical training, bas ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Glycogen Synthase
Glycogen synthase (UDP-glucose-glycogen glucosyltransferase) is a key enzyme in glycogenesis, the conversion of glucose into glycogen. It is a glycosyltransferase () that catalyses the reaction of UDP-glucose and (1,4--D-glucosyl)n to yield UDP and (1,4--D-glucosyl)n+1. Structure Much research has been done on glycogen degradation through studying the structure and function of glycogen phosphorylase, the key regulatory enzyme of glycogen degradation. On the other hand, much less is known about the structure of glycogen synthase, the key regulatory enzyme of glycogen synthesis. The crystal structure of glycogen synthase from '' Agrobacterium tumefaciens'', however, has been determined at 2.3 A resolution. In its asymmetric form, glycogen synthase is found as a dimer, whose monomers are composed of two Rossmann-fold domains. This structural property, among others, is shared with related enzymes, such as glycogen phosphorylase and other glycosyltransferases of the GT-B superf ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Acid Alpha-glucosidase
Acid alpha-glucosidase, also called α-1,4-glucosidase and acid maltase, is an enzyme () that helps to break down glycogen in the lysosome. It is functionally similar to glycogen debranching enzyme, but is on a different chromosome, processed differently by the cell and is located in the lysosome rather than the cytosol. In humans, it is encoded by the ''GAA'' gene. Errors in this gene cause glycogen storage disease type II (Pompe disease). Function This gene encodes lysosomal alpha-glucosidase, which is essential for the degradation of glycogen to glucose in lysosome A lysosome () is a membrane-bound organelle found in many animal cells. They are spherical vesicles that contain hydrolytic enzymes that can break down many kinds of biomolecules. A lysosome has a specific composition, of both its membrane prot ...s. Different forms of acid alpha-glucosidase are obtained by proteolytic processing. Defects in this gene are the cause of glycogen storage disease II, also known a ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Pompe Disease
Glycogen storage disease type II, also called Pompe disease, is an autosomal recessive metabolic disorder which damages muscle and nerve cells throughout the body. It is caused by an accumulation of glycogen in the lysosome due to deficiency of the lysosomal acid alpha-glucosidase enzyme. It is the only glycogen storage disease with a defect in lysosomal metabolism, and the first glycogen storage disease to be identified, in 1932 by the Dutch pathologist J. C. Pompe. The build-up of glycogen causes progressive muscle weakness (myopathy) throughout the body and affects various body tissues, particularly in the heart, skeletal muscles, liver and the nervous system. Signs and symptoms Newborn The infantile form usually comes to medical attention within the first few months of life. The usual presenting features are cardiomegaly (92%), hypotonia (88%), cardiomyopathy (88%), respiratory distress (78%), muscle weakness (63%), feeding difficulties (57%) and failure to thrive (50%). ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Glycogen Storage Disease Type II
Glycogen storage disease type II, also called Pompe disease, is an autosomal recessive metabolic disorder which damages muscle and nerve cells throughout the body. It is caused by an accumulation of glycogen in the lysosome due to deficiency of the lysosomal acid alpha-glucosidase enzyme. It is the only glycogen storage disease with a defect in lysosomal metabolism, and the first glycogen storage disease to be identified, in 1932 by the Dutch pathologist J. C. Pompe. The build-up of glycogen causes progressive muscle weakness (myopathy) throughout the body and affects various body tissues, particularly in the heart, skeletal muscles, liver and the nervous system. Signs and symptoms Newborn The infantile form usually comes to medical attention within the first few months of life. The usual presenting features are cardiomegaly (92%), hypotonia (88%), cardiomyopathy (88%), respiratory distress (78%), muscle weakness (63%), feeding difficulties (57%) and failure to thrive (50%). ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Hyperuricemia
Hyperuricaemia or hyperuricemia is an abnormally high level of uric acid in the blood. In the pH conditions of body fluid, uric acid exists largely as urate, the ion form. Serum uric acid concentrations greater than 6 mg/dL for females, 7 mg/dL for men, and 5.5 mg/dL for youth (under 18 years old) are defined as hyperuricemia. The amount of urate in the body depends on the balance between the amount of purines eaten in food, the amount of urate synthesised within the body (e.g., through cell turnover), and the amount of urate that is excreted in urine or through the gastrointestinal tract. Hyperuricemia may be the result of increased production of uric acid, decreased excretion of uric acid, or both increased production and reduced excretion. Signs and symptoms Unless high blood levels of uric acid are determined in a clinical laboratory, hyperuricemia may not cause noticeable symptoms in most people. Development of gout which is a painful, short-term disorder is ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Lactic Acidosis
Lactic acidosis is a medical condition characterized by a build-up of lactate (especially -lactate) in the body, with formation of an excessively low pH in the bloodstream. It is a form of metabolic acidosis, in which excessive acid accumulates due to a problem with the body's oxidative metabolism. Lactic acidosis is typically the result of an underlying acute or chronic medical condition, medication, or poisoning. The symptoms are generally attributable to these underlying causes, but may include nausea, vomiting, Kussmaul breathing (laboured and deep), and generalised weakness. The diagnosis is made on biochemical analysis of blood (often initially on arterial blood gas samples), and once confirmed, generally prompts an investigation to establish the underlying cause to treat the acidosis. In some situations, hemofiltration (purification of the blood) is temporarily required. In rare chronic forms of lactic acidosis caused by mitochondrial disease, a specific diet or dichloro ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Growth Failure
Failure to thrive (FTT), also known as weight faltering or faltering growth, indicates insufficient weight gain or absence of appropriate physical growth in children. FTT is usually defined in terms of weight, and can be evaluated either by a low weight for the child's age, or by a low rate of increase in the weight. The term "failure to thrive" has been used in different ways, as there is no objective standard or universally accepted definition for when to diagnose FTT. One definition describes FTT as a fall in one or more weight centile spaces on a World Health Organization (WHO) growth chart depending on birth weight or when weight is below the 2nd percentile of weight for age irrespective of birth weight. Another definition of FTT is a weight for age that is consistently below the 5th percentile or weight for age that falls by at least two major percentile lines on a growth chart. While weight loss after birth is normal and most babies return to their birth weight by three wee ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
SLC37A4
Glucose-6-phosphate exchanger SLC37A4, also known as glucose-6-phosphate translocase, is an enzyme that in humans is encoded by the ''SLC37A4'' gene In biology, the word gene (from , ; "...Wilhelm Johannsen coined the word gene to describe the Mendelian units of heredity..." meaning ''generation'' or ''birth'' or ''gender'') can have several different meanings. The Mendelian gene is a ba .... See also * Solute carrier family References Further reading * * * * * * * * * * * * * * * * * * Solute carrier family {{membrane-protein-stub ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
G6PC
Glucose-6-phosphatase, catalytic subunit (glucose 6-phosphatase alpha) is an enzyme that in humans is encoded by the ''G6PC'' gene. Glucose-6-phosphatase is an integral membrane protein of the endoplasmic reticulum that catalyzes the hydrolysis of D-glucose 6-phosphate to D-glucose and orthophosphate. It is a key enzyme in glucose homeostasis, functioning in gluconeogenesis and glycogenolysis. Defects in the enzyme cause glycogen storage disease type I (von Gierke disease). Interactive pathway map See also * G6PC2 * G6PC3 * glucose 6-phosphatase * glycogen storage disease type I References Further reading * * * * * * * * * * * * * * * * * * * {{refend ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Glucose-6-phosphatase
The enzyme glucose 6-phosphatase (EC 3.1.3.9, G6Pase; systematic name D-glucose-6-phosphate phosphohydrolase) catalyzes the hydrolysis of glucose 6-phosphate, resulting in the creation of a phosphate group and free glucose: : D-glucose 6-phosphate + H2O = D-glucose + phosphate Glucose is then exported from the cell via glucose transporter membrane proteins. This catalysis completes the final step in gluconeogenesis and therefore plays a key role in the homeostatic regulation of blood glucose levels. Glucose 6-phosphatase is a complex of multiple component proteins, including transporters for G6P, glucose, and phosphate. The main phosphatase function is performed by the glucose 6-phosphatase catalytic subunit. In humans, there are three isozymes of the catalytic subunit: glucose 6-phosphatase-α, encoded by G6PC; IGRP, encoded by G6PC2; and glucose 6-phosphatase-β, encoded by G6PC3. Glucose 6-phosphatase-α and glucose 6-phosphatase-β are both functional phosphohydrola ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |
Von Gierke's Disease
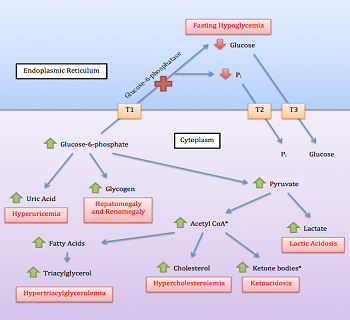
Glycogen storage disease type I (GSD I) is an inherited disease that results in the liver being unable to properly break down stored glycogen. This impairment disrupts the liver's ability to break down stored glycogen that is necessary to maintain adequate blood sugar levels. GSD I is divided into two main types, GSD Ia and GSD Ib, which differ in cause, presentation, and treatment. GSD Ia is caused by a deficiency in the enzyme glucose-6-phosphatase, while GSD Ib is caused a deficiency in the enzyme glucose-6-phosphate translocase. Since glycogenolysis is the principal metabolic mechanism by which the liver supplies glucose to the body during periods of fasting, both deficiencies cause severe low blood sugar and, over time, excess glycogen storage in the liver and (in some cases) the kidneys. GSD I patients typically present with an enlarged liver from non-alcoholic fatty liver disease as the result of this glycogen buildup. Other functions of the liver and kidneys are initiall ... [...More Info...] [...Related Items...] OR: [Wikipedia] [Google] [Baidu] |